Gastric Sleeve Complications

Gastric sleeve complications are rare, but it is important to understand the potential risks before you give your consent to the surgery. Gastric sleeve surgery is currently the most popular bariatric procedure because of its high success rates and minimal risk of serious complications. In particular, after the introduction of laparoscopic technique in 1999, the surgical risks of gastric sleeve have reduced further.
Make an Informed Decision
With more than 300 million adults suffering from obesity globally, gastric sleeve surgery has emerged as a life-saver for millions of patients. You need to work with a weight loss surgeon who understands the potential gastric sleeve complications and risks and explains them to you clearly prior to the procedure. While the benefits of the surgery far outweigh the risks, you should make a judicious choice after consulting a trusted surgeon.
Select an Experienced Surgeon
The high safety profile of gastric sleeve notwithstanding, it is a complex surgery and should only be performed a qualified and experienced bariatric surgeon. Your risk of gastric sleeve complications during and after the surgery will significantly reduce when your operating surgeon, anesthesia team, and the hospital or clinic have a proven track record of safety and success with this surgery.
Gastric sleeve complication rate
Gastric sleeve complication rate is as low as 2.2%, according to a research study published in the prestigious Journal of the American Medical Association (JAMA). The study analyzed the results of 15,275 bariatric surgeries. Researchers found that although 7% of the patients experienced at least one post-operative concern, most were wound related issues or other minor complications. The serious complication rate for gastric sleeve was only 2.2%.
Studies Highlighted by the ASMBS
The American Society for Metabolic and Bariatric Surgery (ASMBS) published the results of two studies to assess the gastric sleeve complication rate. It cited a Stanford University study that found a serious complication rate of 0.96% (within 30 days of surgery). Another study by Cleveland Clinic concluded that gastric sleeve complication and revision rates are the lowest among major bariatric procedures.
NIH Study Analyzes 5-Year Outcomes
A prospective study published by the NIH evaluated the post-surgical mortality, morbidity, and weight loss results of patients who had undergone gastric sleeve surgery. Five years of follow-up study showed that the mortality rate in the study group was 0%. Leakage of staple line occurred in 1.2% of the patients, 0.6% developed pneumonia, 0.6% experienced gastric stricture, and 1.2% reported wound infection.
Gastric sleeve complications during surgery
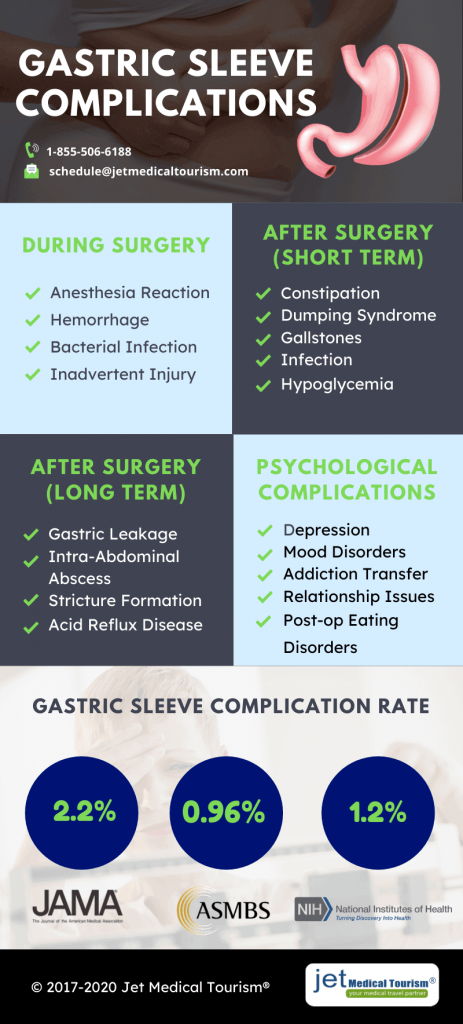 Gastric sleeve complications during surgery may occur in rare cases. A skilled bariatric surgeon and their support team can minimize the risks. Nevertheless, you should be aware of the potential complications that could occur in the surgery room.
Gastric sleeve complications during surgery may occur in rare cases. A skilled bariatric surgeon and their support team can minimize the risks. Nevertheless, you should be aware of the potential complications that could occur in the surgery room.
- Anesthesia Reaction: In rare cases, the patient may have an adverse anesthesia reaction during the surgery. If you suffer from obstructive sleep apnea (OSA), you could experience breathing difficulties while you are unconscious under the influence of anesthesia. A qualified anesthesiologist should be present in the operating room throughout to monitor your condition.
- Hemorrhage: This is one of the potentially serious gastric sleeve complications during surgery that your treatment provider should inform you about. A severe bleeding from the surgical wound can be risky. An experienced surgeon will make advance arrangements for emergency blood transfusion if a serious hemorrhage occurs during the surgical procedure.
- Bacterial Infection: In rare circumstances, you may contract a bacterial tissue infection in the operating room. A systemic infection can be serious and cause a septic shock. Make sure you choose a reputable hospital or bariatric clinic, which can provide a completely sterile surgical environment. Antibiotics prior to the surgery will also reduce your risk.
- Inadvertent Injury: An accidental or iatrogenic injury is a potential gastric sleeve complication during surgery. This may cause tissue damage, but in rare cases, nerve damage may also occur because of an inadvertent surgical injury. Experienced surgeons who have performed hundreds or thousands of gastric sleeve procedures will nearly eliminate this surgical risk.
Gastric sleeve complications – Short term
Just like any other surgery, gastric sleeve also entails the risk of short term or transient complications. In many cases, these concerns will resolve quickly with medical intervention from a physician or surgeon.
- Constipation: This condition may occur in a number of patients after gastric sleeve surgery. Choose a high fiber diet, but avoid granular fibers to avoid bowel obstructions. If the condition persists, talk to your physician.
- Dumping Syndrome: If you eat too much, eat fast, or choose sugary and fatty foods, you may face dumping syndrome, a short term gastric sleeve complication. It may result in vomiting and nausea. You can recover by following your diet plan.
- Gallstones: When you go through rapid weight loss after your gastric sleeve surgery, you may develop gallstones. These are often harmless, but in some cases, they may cause abdominal pain, which will require surgical removal.
- Infection: One of the common gastric sleeve complications in the short term is bacterial infection at the wound site. You should protect the incision areas from contamination for at least three weeks to eliminate this risk.
- Hypoglycemia: Hypoglycemia or low blood sugar may occur in some patients after a gastric sleeve surgery. In the first few months, you will have a stringent diet plan, which could contribute to this condition in rare cases.
Gastric sleeve long term complications
Gastric sleeve long term complications are rare, but they can pose serious health risks. Make sure that you follow the prescribed dietary best practices throughout and visit your surgeon for periodic follow-up appointments. With a healthy and active lifestyle, you can minimize your risk of serious gastric sleeve long term complications. Here are the major complications to watch out for.
Leakage in the Staple Line
Gastric leakage in the staple line is one of the dreaded long term complications following laparoscopic vertical sleeve surgery. According to some researchers, up to five percent of the patients may experience this condition at some point. Depending on when the condition is diagnosed, this complication will be classified as early or delayed.
Patients with co-morbidities such as type 2 diabetes or sleep apnea are a higher risk of a gastric leak. To address the condition, you may require surgical repair along with an abdominal washout. Surgical fluid drainage and administering of antibiotics through IV may also be advised in case of a delayed staple line leak.
Intra-Abdominal Abscess
Another possible gastric sleeve long term complication is the formation of intra-abdominal abscesses. The early symptoms of this condition may include vomiting, nausea, fever and chills, and abdominal pain. Do not ignore these symptoms if the condition does not resolve with diet changes or over the counter medications.
If your doctor has a clinical suspicion that an abscess may have formed in the abdomen, they may order an abdominal CT scan to identify the condition. Treatment of this complication may include antibiotics and percutaneous drainage. The rate of occurrence of this complication is about 0.7%.
Stricture Formation
One of the acute gastric sleeve long term complications is formation of stricture. In some patients, the condition may present acutely because of tissue edema, while in others it may develop in a delayed manner. Common symptoms of stricture include dysphagia, vomiting, nausea, and food intolerance.
The condition may be diagnosed with an upper gastrointestinal endoscopy. Treatment may include a conservative approach, such as rehydration with IV fluids, bowel rest (no eating by mouth), and clinical observation. Endoscopic dilation may be necessary if the conservative therapies fail to resolve symptoms.
YOU MIGHT ALSO LIKE: Long term effects of gastric sleeve
Acid Reflux Disease
GERD or acid reflux is another common long term gastric sleeve complication. Nearly half of the patients who experience GERD will report heartburn as the main symptom, while about one-third will experience regurgitation. GERD occurs when the acid in the stomach reverse flows back to the esophagus, causing irritation to the esophagus lining.
If the symptoms are mild, the condition can be corrected with oral medications and lifestyle changes. Close medical follow up may be necessary in case of moderate acid reflux. If the condition does not resolve even with strong medications, it may be necessary to perform surgery in order to eliminate or ease the symptoms.
Other Long Term Complications
Other gastric sleeve long term complications may occur in some patients, depending on various factors such as age, health, heredity, co-morbidities, and commitment to prescribed diet and exercise. Smoking and alcohol use may also add to the complications in a few cases. Early diagnosis and appropriate treatment is the key to resolving most of these complications, which may include:
- Nutritional deficiency
- Marginal ulceration
- Gallstone disease
- Stomach perforation
- Bleeding in the ulcers
- Internal hernia
- Small bowel obstruction
- Emotional and psychological complications
Psychological complications after gastric sleeve
Although emotional well-being of most patients will improve after weight loss surgery, in rare cases the reverse may happen. You should be aware of the potential psychological complications after gastric sleeve and how these may affect your life and relationships.
- Mood Disorders and Depression: Researchers have found that a few patients who attained substantial relief from mood and depressive disorders in the first two years again developed higher anxiety and depression scores thereafter. Reasons for this occurrence remain unclear.
- Higher Rate of Suicides: Some patients who had a history of psychological disorders or depression prior to the surgery may continue to be a higher risk of suicide even after their gastric sleeve. While this occurrence is extremely rare, it is vital to address mental health issues promptly.
- Post-op Eating Disorders: One of the more common psychological complications after gastric sleeve surgery is the development of eating disorders. Some patients may be diagnosed with night eating syndrome, while some others may suffer from binge eating disorder post-surgery.
- Addiction Transfer: When a patient is not able to use food as an escape from their emotional challenges, they may be more vulnerable to a phenomenon called “addiction transfer.” Addiction to tobacco, drugs, alcohol, or sex may occur in a few cases after gastric sleeve surgery.
- Relationship Issues: Psychological gastric sleeve complications may sometimes lead to challenges in the marital relationship. A partner may start feeling unwanted or jealous, or the dynamics of the relationship may change because the patient is going to psychological problems post-surgery.
Gastric sleeve Mexico complications
Gastric sleeve Mexico complications are rare, especially when the procedure has been performed by a well-qualified bariatric surgeon. However, the possibility of post-operative side effects and complications cannot be ruled out. When the complications arise, they could range from temporary or short term concerns to serious and potential life threatening issues.
Acute vs. Chronic Complications
Gastric sleeve Mexico complications can be classified as acute and chronic, depending on the timing and nature of the problem. Acute complications will typically arise shortly after the procedure, and may include pain, bleeding, clotting, and gastric leaks. Chronic complications, on the other hand, may develop several months after the surgery, and may persist for a longer time. These may include strictures, ulcers, gallstones, and nutrition deficiencies.
Minimize Your Risk of Complications
You can significantly reduce your risk of gastric sleeve Mexico complications if you diligently abide by your surgeon’s instructions. Remember that even the most successful gastric sleeve surgery is not a magic bullet. You will need to follow the prescribed dietary guidelines, pursue a fitness regimen, take your medications and supplements on time, and visit your surgeon for follow-up appointments. A balanced lifestyle will help you minimize your risk of complications.
Signs of gastric sleeve complications
Your body will give you distress signals if an acute or chronic gastric sleeve complication is developing after the surgery. Some of these signs and symptoms are easy to identify. You should take them seriously and consult with your physician or surgeon, particularly if the condition seems to persist or worsen.
- Pain or Fever: If you experience abnormal pain in the incision sites, which does not resolve with pain medications, it could be a sign of infection. In some cases, you may also develop mild fever which keeps coming back. This condition may occur within the first few days of your surgery.
- Dyspepsia: Mild indigestion, bloating or upset stomach may be a temporary after-effect of gastric sleeve surgery. However, if the symptoms become severe or fail to resolve with over the counter medications, it could be one of the signs of gastric sleeve complications.
- Diarrhea: Following your gastric sleeve surgery, it is possible to have mild bouts of diarrhea due to changes in the gut biome. However, if the condition persists for a longer duration, you should see a gastroenterologist or bariatric surgeon to determine if you have other complications.
- Abdominal Pain: Up to 50 percent of all emergency room visits and post-surgical complaints after a gastric sleeve surgery are related to abdominal pain. If the pain is persistent or frequent, the condition requires a careful diagnosis because it could be a sign of gastric sleeve complications.
Late complications of gastric sleeve
 In some cases, even if the gastric sleeve surgery goes as planned and the patient recovers with minimal downtime and side effects, complications may occur after a few years. Here are some of the late complications of gastric sleeve that you should watch out for.
In some cases, even if the gastric sleeve surgery goes as planned and the patient recovers with minimal downtime and side effects, complications may occur after a few years. Here are some of the late complications of gastric sleeve that you should watch out for.
- Continuance of Co-morbidities: You may have undergone sleeve gastrectomy to obtain relief from obesity-related medical conditions, such as diabetes or sleep apnea. But in a few cases, the symptoms of these co-morbidities may come back months or years later.
- Acid Reflux Disease (GERD): Gastroesophageal reflux disease or GERD may occur in a number of patients within a few years. This is one of the common late complications of gastric sleeve surgery. Symptoms include heartburn, bloating, upset stomach, and a feeling of fullness.
- Peptic Ulcers: Peptic ulcers, commonly known as stomach ulcers, may sometimes develop at a late stage after your VSG procedure. Symptoms include blood in stools and vomit or abdominal pain. Your doctor will diagnose this condition by performing an upper endoscopy.
- Stomach Obstruction: One of the rare gastric sleeve late complications is stomach obstruction. Narrowing and scarring of the stomach outlet (a phenomenon called stenosis) may sometimes make it hard to digest food. Your surgeon can correct this condition by stretching the narrowed area.
Tips to avoid complications after gastric sleeve surgery
The risk of complications after gastric sleeve surgery can be avoided or mitigated with your own efforts. Any surgery has some risks associated with it, but if you take the right steps from the beginning of your weight loss journey, you will be able to avoid most of the risks and complications after gastric sleeve.
- Make a decision to undergo gastric sleeve surgery at an early age as far as possible when your body is more resilient and strong.
- Choose a competent bariatric surgeon who has a proven track record of successful gastric sleeve surgeries.
- Work towards moderate eating and mild exercises even before your scheduled surgery and follow your pre-op diet plan diligently.
- Avoid strenuous physical activities or aggressive exercises for the first two to three months after your gastric sleeve surgery.
- Stick to your recommended post-op diet and exercise plan even when you hit a weight loss plateau or experience stress or other issues.
- Follow a healthy and balanced lifestyle, and avoid tobacco, alcohol, and intoxicating substances as far as possible.
- Sleep well, drink adequate water to stay hydrated, and take your supplements on time to minimize complications after gastric sleeve.
- Visit your physician or surgeon for your scheduled medical appointments and do not hide any signs or symptoms of distress.
Gastric sleeve complications death
Some patients are worried about gastric sleeve complications death, and may feel reluctant to undergo the procedure. But the good news is that the 30-day mortality rate of gastric sleeve surgery is extremely low. In any surgical procedure, the risk of death is highest during or just after the surgery when acute complications may occur. Therefore, researchers focus on the 30-day mortality rate to determine the risk.
Negligible Death Rate after VSG
The NIH published a research study of 6,118 patients who received different bariatric surgery procedures. Within 30 days after the procedure, 18 patients died, indicating a mortality rate of 0.3%. However, out of these 18 patients, 16 had received other procedures, while only 2 patients had undergone gastric sleeve. This indicates that gastric sleeve complications death rate is extremely low or negligible.
Higher Risk in Case of Extreme Obesity
In the aforementioned NIH study, researchers determined that the two patients who died after gastric sleeve surgery were both suffering from extreme obesity. Their BMI was 51.7 and 62.9 respectively. In other words, both patients were suffering from Class 5 obesity, which is the extreme stage. In both cases, the surgeons had planned gastric sleeve only as the first stage of a 2-stage bariatric surgery.
Gastric sleeve complication stories
Myths and misconceptions about gastric sleeve surgery abound, but they should not deprive you of your chance to restore your health and quality of life. Some of the gastric sleeve complication stories of past patients can be scary, but you should view them objectively. The benefits of gastric sleeve will far outweigh the risks and in almost every case, you are safer undergoing the surgery rather than avoiding it.
When you learn about gastric sleeve complication stories of other patients, you should check the patient’s age, BMI, and health condition and compare them with your parameters. You should also seek to know the cause of the complications, and whether the patient followed surgeon’s advice post-operatively. Talk to a trusted bariatric surgeon who will evaluate your unique risk profile and make the best recommendation for your surgery.
CHECK THIS OUT: Why am I not losing weight after gastric sleeve surgery? Common myth debunked!
Gastric sleeve complications smoking
Although occasional smoking may not harm your prospects as a sleeve gastrectomy candidate, but regular smoking may increase your risks. The right approach would be to clearly inform your surgeon about your smoking habit so that they correctly determine whether you qualify for VSG. Gastric sleeve complications smoking can be minimized if you follow your surgeon’s advice.
Your surgeon may instruct you to stop smoking at least temporarily for a few weeks before and after your sleeve gastrectomy. Nicotine in tobacco smoke can interfere with your oxygen flow and pose risks during surgery as well as post-op healing. Talk to your surgeon about gastric sleeve complications smoking at your first consultation and go by their recommendation.
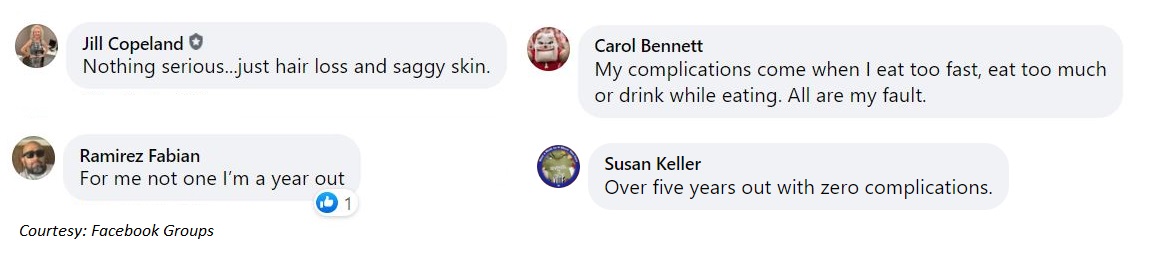
Gastric sleeve complications- Real Patient Reviews
We participated in a few bariatric support groups on Facebook and asked patients if they have faced any complications after gastric sleeve surgery. Read what they have to say about it:
Final words on gastric sleeve complications
Gastric sleeve surgery is a life-changing procedure that can dramatically improve your health and fitness levels and increase your longevity. Like any other surgery, it is possible to experience minor or major gastric sleeve complications in rare cases. But the important question for you to evaluate is whether you are a higher risk with the surgery or without the surgery?
Living with obesity not only reduces your quality of life, but also increases your risk of life-threatening diseases. Leading medical associations worldwide recommend weight loss surgery as a credible option to eliminate obesity. When you choose the right surgeon and stay committed to a healthy lifestyle, your risk of gastric sleeve complications will probably be lower than any other general life and health risks.
Other articles on gastric sleeve surgery
- Gastric sleeve incisions, illustrations
- Gastric sleeve before and after pictures: Best photos
- Finding gastric sleeve surgeons: A step by step guide
- Gastric sleeve regrets
- Gastric bypass weight loss chart, timeline 2020
- Gastric sleeve reviews
- Gastric sleeve procedure for weight loss
- Vertical sleeve gastrectomy procedure: Cost, diet, recovery, success stories
- How much does gastric sleeve cost?
- What is the success rate of gastric sleeve?
References:
- Deitel M. Overweight and obesity worldwide now estimated to involve 1.7 billion people. Obes Surg. 2003;13:329–30.
- Frezza EE. Laparoscopic vertical sleeve gastrectomy for morbid obesity. The future procedure of choice? Surg Today. 2007;37:275–81.
- Marceau P, Hould FS, Simard S, et al. Biliopancreatic diversion with duodenal switch. World J Surg. 1998;22:947–54.
- Moon Han S, Kim WW, Oh JH. Results of laparoscopic sleeve gastrectomy (LSG) at 1 year in morbidly obese Korean patients. Obes Surg. 2005;15:1469–75.
- Melissas J, Koukouraki S, Askoxylakis J, et al. Sleeve gastrectomy: A restrictive procedure? Obes Surg. 2007;17:57–62.
- Uglioni B, Wolnerhanssen B, Peters T, et al. Midterm results of primary versus secondary laparoscopic sleeve gastrectomy (LSG) as an isolated operation. Obes Surg. 2009;19:401–6.
- Cottam D, Qureshi F, Mattar S, et al. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc. 2006;20:859–63.
- Parikh A, Alley JB, Peterson RM, et al. Management options for symptomatic stenosis after laparoscopic vertical sleeve gastrectomy in the morbidly obese. Surg Endosc. 2012;26:738–46.
- Gehrer S, Kern B, Peters T, et al. Fewer nutrient deficiencies after laparoscopic sleeve gastrectomy (LSG) than after laparoscopic Roux-en-Y-gastric bypass (LRYGB) — a prospective study. Obes Surg. 2010;20:447–53.
- Sundbom M, Karlson BM. Low mortality in bariatric surgery 1995 through 2005 in Sweden, in spite of a shift to more complex procedures. Obes Surg. 2009;19:1697–1701.
- Lancaster RT, Hutter MM. Bands and bypasses: 30-day morbidity and mortality of bariatric surgical procedures as assessed by prospective, multi-center, risk-adjusted ACS-NSQIP data. Surg Endosc. 2008;22:2554–2563.
- DeMaria EJ. “Bariatric Surgery for Morbid Obesity,” New England Journal of Medicine (May 24, 2007): Vol. 356, No. 21, pp. 2176–83.
- Wadden TA, et al. “Psychosocial and Behavioral Status of Patients Undergoing Bariatric Surgery: What to Expect Before and After Surgery,” Medical Clinics of North America (May 2007): Vol. 91, No. 3, pp. 451–69.