Acid Reflux or GERD After Gastric Sleeve

Does gastric sleeve surgery cause gastroesophageal reflux disease (GERD)? Researchers have struggled to find a conclusive answer to this question in recent years, but different studies continue to show diverging results. Some studies have indicated a higher incidence of GERD after gastric sleeve, while the others have shown the exact opposite: a reduced incidence after the VSG surgery.
According the experts at the UCLA, many patients report a relief from acid reflux after gastric sleeve. During the procedure, the bariatric surgeon should make sure that no fundus (upper stomach portion) is left inside when the partial stomach removal is performed. Experience surgeons are aware of the potential GERD complications, and will take care to minimize the risk.
Contact Jet Medical Tourism® today.
What is GERD or Gastroesophageal Reflux Disease?
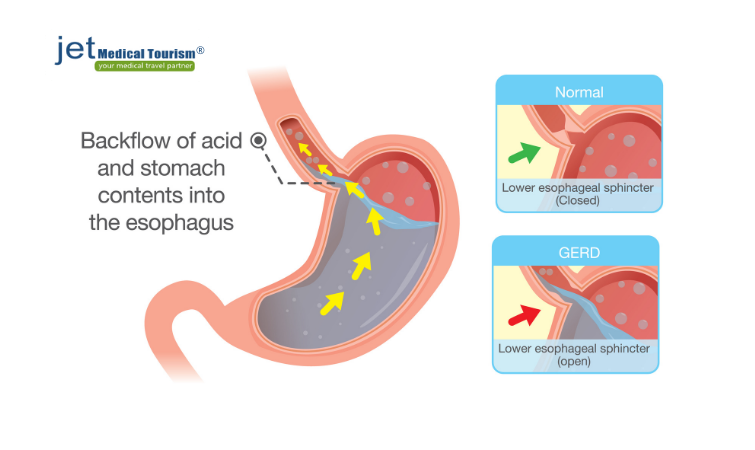
Gastroesophageal reflux disease (GERD), commonly known as acid reflux, occurs when your digestive system develops the tendency to create a backflow of stomach acid into the esophagus (which connects your mouth to the stomach). Gastric sleeve acid reflux may occur in some patients after the surgery. On the other hand, some other patients with a pre-existing GERD may find relief from the symptoms after their gastric sleeve surgery.
How Frequently GERD May Occur Post-Surgery?
Patients who develop GERD after gastric sleeve may typically experience the condition two or more times a week in a mild form. More severe forms of acid reflux may generally occur only about once a week. Management of GERD after sleeve gastrectomy is usually possible with diet and lifestyle adjustments. Some patients may require over the counter or prescription medications to treat the symptoms.
How Acid Reflux after Gastric Sleeve Occurs?
Although the research remains controversial on this issue, gastric sleeve surgery and acid reflux may have some correlation. During the sleeve gastrectomy, nearly 80% of the stomach volume is removed. This causes substantial anatomical changes to your stomach and esophagus, which may contribute to the occurrence of GERD in some patients. However, weight loss and health post-op diet can mitigate the symptoms in most cases.
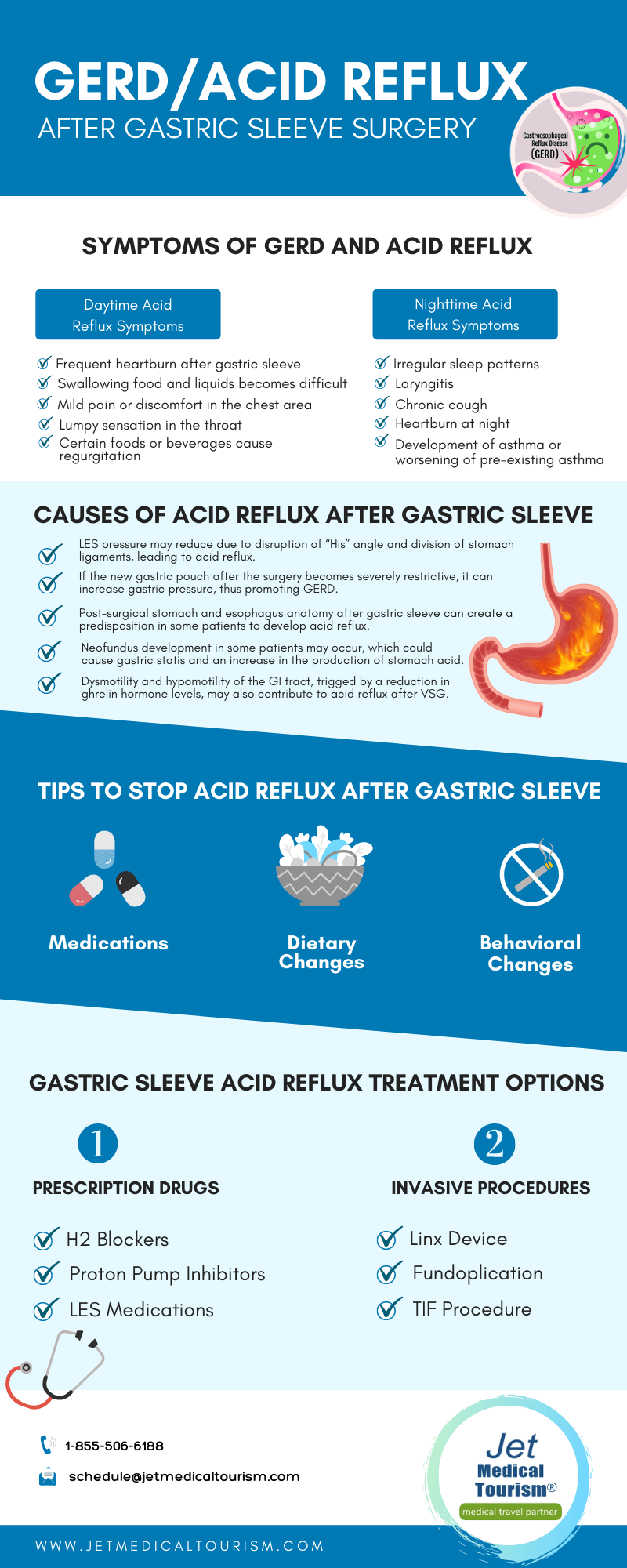
Symptoms of GERD and Acid Reflux
You may be suffering from GERD after gastric sleeve if you exhibit the following signs and symptoms frequently:
Daytime Acid Reflux Symptoms
- Frequent heartburn after gastric sleeve
- Swallowing food and liquids becomes difficult
- Mild pain or discomfort in the chest area
- Lumpy sensation in the throat
- Certain foods or beverages cause regurgitation
Nighttime Acid Reflux Symptoms
- Irregular sleep patterns
- Laryngitis
- Chronic cough
- Development of asthma or worsening of pre-existing asthma
- Heartburn at night
Risk Factors of GERD after VSG Surgery
- Drinking carbonated, caffeinated, or alcoholic beverages
- Regular use of blood thinning drugs or NSAIDs
- Food triggers, such as processed, fried, or high-fat foods
- Eating late at night or consuming large meal portions
- Regular smoking
Acid reflux or GERD after gastric sleeve
A research report published in an eminent journal sheds light on both dimensions of how acid reflux after gastric sleeve may increase or decrease. Considering these directly opposing conclusions, patients should not feel discouraged about undergoing their weight loss surgery. Here is what the two different sets of research show:
Increase in GERD after Sleeve Gastrectomy
Some research studies show that your post-surgical anatomy after VSG may predispose you to acid reflux disease. During the gastric sleeve surgery, the “His” angle (which acts a protective shield against GERD) gets destroyed or disrupted. This may contribute to the increase in acid reflux symptoms in the months following your surgery. Some researchers also indicate that increased gastric pressure after VSG may trigger increased acid reflux.
Decrease in GERD after Sleeve Gastrectomy
Another set of research studies shows that up to 20 percent of the patients with pre-existing GERD symptoms experienced reduction in their symptoms after their gastric sleeve surgery. Removal of the fundus leads to elimination of most of the parietal cells in your stomach. These are acid generating cells, and their removal after VSG may contribute to a reduction in the production of gastric acid.
Heartburn after gastric sleeve
Heartburn, as the name suggests, is a burning sensation that may occur in your chest. The condition is often accompanied by a bitter aftertaste in the mouth or throat. Heartburn after sleeve gastrectomy occurs more commonly when you eat larger meal portions than what your nutritionist prescribed, or include the wrong foods in your diet that are hard to digest.
What Causes Heartburn after Sleeve Surgery
Heartburn usually occurs when the food you eat does not retain in the stomach and backs up into the tube that carries the food from the mouth to the stomach. The function of this tube called esophagus may get disturbed in some cases after gastric sleeve surgery. When the acids from the stomach irritate the esophagus lining, it may cause heartburn.
Can Hiatal Hernia Cause Heartburn?
Some patients may develop a complication called hiatal hernia following their gastric sleeve surgery. This may sometimes contribute to the symptoms of heartburn. When the condition is minor, it will generally not cause trouble and you may not even know about it. But when a large hiatal hernia occurs, it may cause the stomach acid to back up into your esophagus, resulting in heartburn.
Heartburn vs Acid Reflux vs GERD
Symptoms of heartburn, acid reflux, or GERD after gastric sleeve may occur in some patients. While most people use all three terms interchangeably, there are subtle but significant differences between them.
| Heartburn | Acid Reflux | GERD |
| Heartburn after gastric sleeve may develop in your esophagus. The condition is marked by mild or sharp pain in the chest, but it has nothing to do with your cardiac health. When the stomach acid backs up in the esophagus, it can create a burning or irritating sensation in the sensitive lining of the esophagus. This may cause the symptoms of heartburn and tightness in the chest. | The stomach and the esophagus are connected by the lower esophageal sphincter muscle (LES). This circular muscle performs the role of shutting the esophagus opening once the food has been delivered to the stomach. Acid reflux after gastric sleeve may occur when the LES functioning is disrupted during the surgery. It may not shut the opening properly, causing the acid to move back from the stomach. | When the acid reflux condition becomes chronic, it is called GERD. GERD after VSG may be marked by an inflamed esophagus or frequent occurrence of acid reflux. Poor dietary practices or lying down right after eating may sometimes contribute to GERD symptoms after your surgery. Management of GERD after sleeve gastrectomy is vital to minimize the risk of permanent damage to your esophagus. |
What causes acid reflux after gastric sleeve?
Some research studies have indicated the development of de novo (new) acid reflux after gastric sleeve as well as intensified symptoms of pre-existing acid reflux in certain patients. Here are some of the potential causes of gastric sleeve acid reflux as indicated by various researchers:
- LES pressure may reduce due to disruption of “His” angle and division of stomach ligaments, leading to acid reflux.
- If the new gastric pouch after the surgery becomes severely restrictive, it can increase gastric pressure, thus promoting GERD.
- Post-surgical stomach and esophagus anatomy after gastric sleeve can create a predisposition in some patients to develop acid reflux.
- Neofundus development in some patients may occur, which could cause gastric statis and an increase in the production of stomach acid.
- Dysmotility and hypomotility of the GI tract, trigged by a reduction in ghrelin hormone levels, may also contribute to acid reflux after VSG.
How to stop acid reflux after gastric sleeve
Gastric sleeve acid reflux treatment can be performed using different approaches, depending on the severity of your symptoms. Your bariatric surgeon will look at your medical history and evaluate your current symptoms to determine a diagnosis. In general, the following three approaches may be adopted to help stop acid reflux after gastric sleeve:
- Medications: Your surgeon may advise the appropriate antacids that will help neutralize the stomach acid. Another commonly used medication is H2 blockers, which will start working before the stomach acid formation actually occurs. In a few cases, PPI or proton pump inhibitors may be prescribed, which act faster and stronger to counter stomach acid.
- Dietary Changes: Management of GERD after sleeve gastrectomy may involve adjustments to your diet. Your surgeon may ask you to avoid the use of trigger foods, such as alcohol, coffee, chocolate, sodas, fatty foods, and spicy foods. You may have to reduce your meal portions in order to mitigate a distended stomach, and avoid late night eating or snacking.
- Behavioral Changes: You may be required to quit or minimize the habit of smoking if you are experienced persistent symptoms of acid reflux after gastric sleeve surgery. Wear loose fitting clothes, do not lie down immediately after eating, sleep with your head in a slightly raised position, and diligently maintain your recommended diet and exercise regimen.
Gastric sleeve acid reflux treatment options
Although there is some controversy about the correlation between gastric sleeve surgery and acid reflux, a small percentage of patients may experience new or worsened symptoms post-operatively. It’s vital to report your symptoms to your surgeon and seek their advice on how to stop acid reflux after gastric sleeve. Here are some of the proven treatment options:
Gastric Sleeve Acid Reflux Treatment – Prescription Drugs
- H2 Blockers: Prescription strength H2 blockers may include drugs, such as nizatidine and famotidine. Most patients can tolerate these H2 receptor blockers very well, but you should keep a track of your vitamin B12 levels if you use these meds for the long-term.
- Proton Pump Inhibitors: Prescription strength PPI medications include lansoprazole, esomeprazole, omeprazole, rabeprazole, pantoprazole, and dexlansoprazole. Mild side effects, such as nausea, headache, and diarrhea may occur in a few patients with these drugs.
- LES Medications: If your acid reflux condition has occurred because of weakened lower esophageal sphincter (LES) muscle, your surgeon may prescribe medications to strengthen this muscle. Side effects of these meds may include nausea and fatigue in some patients.
Gastric Sleeve Acid Reflux Treatment – Invasive Procedures
- Linx Device: This is an advanced procedure to control the symptoms of GERD after gastric sleeve. Your surgeon will implant a ring of magnetic beads around the point where your esophagus and stomach meet. The magnetic pull will help improve the sphincter muscle function.
- Fundoplication: Your surgeon will wrap the upper portion of your stomach around the sphincter muscle. This will help tighten the weakened muscle and stop the occurrence of acid reflux. This procedure can be performed as a partial or full surgery using a laparoscope for high precision.
- TIF Procedure: TIF or transoral incisionless fundoplication procedure is one of the latest solutions, which creates a partial wrap around the lower part of your esophagus. TIF is performed endoscopically, and no cuts or incisions are involved. Minimal downtime is required with this treatment.
Sleeve to bypass for reflux: Yes or No?
Sleeve to bypass for reflux is a treatment of the last resort when medical management of the serious GERD symptoms fails to work. Your surgeon will evaluate your health factors, the severity of your acid reflux symptoms, and your personal goals before recommended gastric sleeve to gastric bypass revision surgery.
Conversion from Gastric Sleeve to Gastric Bypass
For patients who have had a gastric sleeve surgery, it is usually possible to perform a gastric bypass revision. Gastric bypass is known to be highly effective in resolving or diminishing the symptoms of acid reflux disease. In the revision procedure, no further stomach reduction is usually required. Your surgeon will only reroute the small intestine to complete the bypass.
Conversion from Gastric Sleeve to Mini Gastric Bypass
Sleeve to bypass for reflux becomes much easier if you are a candidate for a mini bypass revision surgery. This procedure is significantly less invasive and minimizes your risk of complications. Mini gastric bypass will avoid intestinal resection. Your surgeon will only pull a small part of the intestine up to the new pouch in order to create a new bypass connection.
Other related issues after VSG surgery
GERD after gastric sleeve is not the only problem patients may face. In some cases, other issues related to the digestive tract may occur. Fortunately, most of the concerns are mild in nature, and can be treated with diet and behavior modifications or over the counter medications. However, if the symptoms persist or cause severe discomfort, you must consult with your bariatric surgeon.
Belching after gastric sleeve
Belching or burping is your body’s way to releasing excessive air that has been trapped in your upper digestive tract. Belching after gastric sleeve surgery is a common problem because of the changes to the stomach. The air may reach your stomach, and may collect in the esophagus. GERD or acid reflux may trigger excessive belching in some cases.
Indigestion after gastric sleeve surgery
The general discomfort you sometimes feel in your upper abdomen is called indigestion or dyspepsia. This is not an illness, but it may be marked by a feeling of fullness even when you haven’t eaten and may sometimes cause abdominal pain. Indigestion after gastric sleeve surgery is common, and can be addressed with medications and lifestyle improvements.
Gastric sleeve ulcer
Gastric ulcers, commonly known as stomach ulcers, are painful sores that may develop in the delicate lining of your stomach. A gastric sleeve ulcer is usually a minor peptic ulcer that can be cured with medications or simply with natural treatments. However, in absence of treatment, the ulcer may become severe and cause significant discomfort.
RELATED ARTICLE: Gastric Sleeve Complications
Hiatal hernia after gastric sleeve
A hiatal hernia after gastric sleeve can be serious and painful complication. However, it is possible to treat it without surgery in most cases. In exceptional situations, you may require surgery, but it is a rather simple procedure with predictable and lasting outcomes. Symptoms of hiatal hernia include chest pain, swallowing difficulty, and shortness of breath.
Abdominal pain after gastric sleeve
Abdominal pain after gastric sleeve surgery may occur due to a number of reasons. Infection, inflammation, intestinal obstruction, or another disorder may cause pain. However, if the pain is progressive and occurs within days or weeks of your surgery, it may have been caused by a perforation or leakage. This may require an urgent corrective surgery.
Gas pain after gastric sleeve surgery
When gas gets trapped in your abdomen or chest, it can feel like a stabbing or stinging pain. Gas pain after gastric sleeve surgery may occur more frequently if you are experiencing acid reflux symptoms. This may cause a gas bubble to be trapped, which will cause pain. It is vital to follow your prescribed post-op VSG diet to minimize your chances of gastric pain.
Conclusion
GERD after gastric sleeve surgery may occur in some cases, but this should not discourage you from going ahead with your procedure. The benefits of weight loss will usually far outweigh the minor potential complications. In fact, many patients also report a sustainable relief from acid reflux and other digestive issues after their sleeve gastrectomy.
To sum up, the jury is still out on whether a VSG will relieve or induce the symptoms of GERD in a patient. The right approach would be to consult with a qualified and experienced bariatric surgeon who can evaluate your health condition objectively, educate you about the pros and cons of gastric sleeve surgery, and help you make a decision that works best for you.

