Pregnancy and Obesity

“What weight is considered obese?” you may ask. Well to many obesity is recognized and measured by calculating a person’s BMI or body mass index, which measures the amount of body fat in proportion to a person’s physique (height & weight) with respect to gender. Many obese women tend to experience difficulty conceiving a child or infertility (are unable to have a baby on their own) and can even experience a greater chance of failure for IVF (in-vitro fertilization) interventions.
However, if you are obese and able to conceive a child that is wonderful as you have overcome obstacles the majority of obese women endure, “but what happens next?” you may ask.
Should you become pregnant and are obese you will most likely have what is called a “high-risk pregnancy”, which requires more intense follow-up prenatal visits and monitoring to ensure the health of the growing fetus and mother the whole nine months. As obesity causes hormonal imbalances in women, obese mothers undergo so many risks, but there is hope with the right types of intervention.
Contact Jet Medical Tourism® today for more information on topics related to obesity.
Pregnancy and obesity: Know the risks
Pregnancy and obesity have many risks that mothers should know about early on to ensure safe delivery. In the US, obesity is an epidemic with more women affected by obesity than compared to men. From an obese mother, babies can come out very small in size, which is most common, but less commonly, can also come out very large in other cases. Another risk is stillbirth delivery in obese mothers.
In women over the age of 40, a mother’s risk for stillbirth goes up even more. Other health risks obese mothers may endure during pregnancy include:
- Preeclampsia (high blood pressure during pregnancy causing organ failure such as kidneys/liver failure; usually comes with a high quantity of protein found in a patient’s urine. Preeclampsia can cause eclampsia/seizures, and even although rare, stroke; typically starts to affect a woman at the 20th week or later in their pregnancy)
- Gestational diabetes (i.e., pregnancy related high blood glucose levels)
- Heart problems
- Sleep apnea (the person stops breathing during sleep)
- Hypertension (i.e., high blood pressure)
- Increased need for C-section (Cesarean delivery; risks for infection/bleeding and delivery complications are increased)
- Miscarriage
What weight is considered obese?
What weight is considered obese depends on the person’s physique and gender, which is calculated by obtaining a BMI (body mass index). To calculate your BMI today, you can click on the following link to better understand where you stand in terms of obesity risk. The CDC or Centers for Disease Control and Prevention describes obesity as belonging to a class depending on your calculated BMI from your weight and height.
The CDC describes a normal BMI of being between 18.5-24 for an average height adult. An overweight BMI is typically 25-29. An obese BMI is 30+. A morbidly obese BLI is 40+. For example, for an adult with a height of 5’9’’ and a weight of 203 pounds+, this would define them as obese with a BMI of 30+.
The CDC’s classes of obesity:
| Class | BMI (range) |
| 1 | 30-34 |
| 2 | 35-39 |
| 3 | 40+ |
SEE THIS: BMI for gastric sleeve surgery
BMI for pregnancy
BMI for pregnancy varies depending on the pregnancy type and mother’s physique (height and weight). The Mayo Clinic recommends for a single pregnancy, a pregnant woman who has a BMI of 30 or greater (BMI is measured in kilograms per meter squared) should aim for a weight gain of only 11-20 pounds throughout her entire pregnancy. However, for a multiple pregnancy in a pregnant woman having a BMI of 30+ with twins or more should aim for gaining anywhere between 25-42 pounds total.
Pregnancy and obesity guidelines

Pregnancy and obesity guidelines include self care methods to limit health risks for mothers and babies. Before pregnancy and during, FIGO or, International Federation of Gynecology and Obstetrics, recommends women calculate their BMI to better understand their risks during pregnancy and take vitamin supplements (specifically folic acid, between 0.4-5 mg) even before one to three months of getting pregnant.
- Before and during pregnancy, a healthy diet and lifestyle are encouraged, but bariatric surgery is recommended for those in urgent need of weight loss intervention which can occur before pregnancy.
- During pregnancy, obese women should continue to visit their healthcare provider as often as recommended to accommodate their specific health situation, including all clinical management services such as diagnostics and fatal monitoring as necessary.
- After pregnancy, post-natal follow-care is needed to access for material or complications in the baby if any should arise.
Obesity and pregnancy complications
Obesity and pregnancy complications are numerous as a pregnant woman’s BMI reaches 30. There are also risks the growing fetus of an obese mother may endure, such as: being prone to a higher risk of obesity themselves in life, birth defects, and even asthma.
- Birth defects caused by obesity can include heart and/or brain defects.
- Babies born to obese mothers may also be delivered pre-term as previously mentioned, requiring increased healthcare support (NICU; or neonatal intensive care unit) after birth.
Morbid obesity and pregnancy complications
Morbid obesity and pregnancy complications are more common as a woman’s BMI increases. For example, in morbid obesity or extreme obesity, this is typically defined as a BMI of 40+, a mother may endure more serious health risks to herself and her growing fetus. Physicians often recommend for pregnant women with a BMI of 40+ to gain a lower amount of weight than the typically recommended amounts for their pregnancy.
- By thus, a morbidly obese pregnant woman can reduce the chances of her baby coming out too large (called macrosomia) and reduce the need for a C-section.
- At the same time, this common recommendation may increase the chances of a morbidly obese mother giving birth to an underweight baby preterm (especially if the mother has pre-eclampsia).
CHECK THIS OUT: Morbid obesity BMI chart: Am I morbidly obese?
Weight loss for pregnancy

Weight loss for pregnancy includes weight loss intervention prior to getting pregnant. Bariatric surgery can be a very effective weight loss intervention for women who are deciding they would like to get pregnant eventually, but would prefer to lose weight first. If you decide to have bariatric surgery, it is recommended to wait between one to two years before becoming pregnant.
Waiting this period of time after bariatric surgery will ensure you achieve the fastest weight loss possible. Furthermore, fertility problems if present may resolve on their own in women after having bariatric surgery!
Due to achieving rapid weight loss, this means bariatric surgery will make it easier for women to get pregnant who previously struggled with fertility in the past. Bariatric surgery also resolves many comorbidities or conditions commonly caused by obesity, such as improving hypertension, obstructive sleep apnea, high cholesterol, and more.
Pregnancy hormone for weight loss
Pregnancy hormone for weight loss, commonly known as HCG, has been used by women with hopes of losing weight with over the counter products containing this hormone. During pregnancy, the hormone HCG or human chorionic gonadotropin hormone is made. With the latest low calorie fad diets going around, women started to use weight loss pill products containing HCG in combination with a very dangerously low calorie diet (500-800 calories per day limit) to lose weight.
- To be clear, the FDA or Food and Drug Administration has strongly advised against this diet and use of any weight loss products containing HCG as they have been proven unsafe.
- In fact, over the counter HCG products are illegal in the US since they are not effective weight loss interventions and serve to increase a person’s risk for cancer.
- Furthermore, HCG over the counter products often cause dangerous side effects such as the formation of gallstones, the blockage of blood vessels (known as a thromboembolism), high risk for blood clot formation, irregular heartbeat, and more negative side effects in consumers.
YOU MIGHT WANT TO READ: Ghrelin vs Leptin: Impact of hunger hormones on obesity
Pregnancy after bariatric surgery: Is it safe?
Pregnancy after bariatric surgery can be safe if proper planning and precautions have been taken. After bariatric surgery, pregnancy should be carefully considered based on a few factors, such as advanced maternal age, time lapse after having bariatric surgery, and if any other obesity related issues/comorbidities (type II diabetes, heart disease, etc.) are present.
- If patients get pregnant too soon after bariatric surgery, they are at a higher risk for developing long-term vitamin and mineral deficiencies (e.g., A, C, D, B6, calcium, phosphorus, iron, etc).
- The Mayo Clinic recommends patients wait 1 year to 1.5 years after having bariatric surgery to become pregnant (for weight stabilization to occur). Experts say waiting even longer, such as 2 years after surgery is even better and safer.
DETAILED READ: Pregnancy after bariatric surgery: Is it healthy and safe?
PCOS and weight loss surgery
PCOS and weight loss surgery can be described with respect to each other as being “the problem and the solution”. The endocrine disorder polycystic ovarian syndrome or PCOS commonly causes obesity in addition to infertility. It can be a problem for women within their reproductive ages.
PCOS causes insulin resistance and defects in insulin secretion. Insulin increases the production of ovarian androgens (male hormones). An excess of androgen has been reported in PCOS and increases in LH (luteinizing hormone) production, which make it difficult for an egg to be released, enhancing infertility.
- Studies have reported gastric bypass surgery to be a very effective treatment option for targeting the symptoms of PCOS.
- PCOS can lead to endometrial cancer and bariatric surgery such as gastric bypass can prevent the development of endometrial cancer.
RELATED READ: Gastric sleeve and PCOS: Everything you need to know
Gastric sleeve and pregnancy
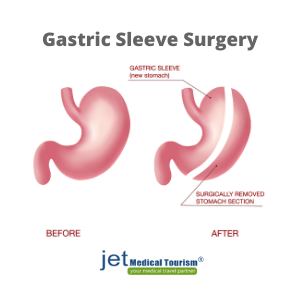
Gastric sleeve and pregnancy when the time is right can allow an obese woman to safely have a baby. Studies in 2019 have shown as early as less than 1 year after having completed gastric sleeve bypass surgery (or even other types of bariatric surgery as well) can not only lower the amount of weight a pregnant woman gains during pregnancy, but also promotes higher weight loss throughout the pregnancy, and leads to less weight retention postpartum. These results were taken when analyzing study participants 6 months postpartum.
- Under short-term analysis, babies born of obese mothers in this study were all reported to have developed the same as any non-obese woman could have birthed them, with normal birth weight and no apparent defects.
- Therefore, having gastric sleeve surgery prior to pregnancy has been shown to improve many pregnancy outcomes.
- Of course, more studies are needed to determine long-term health outcomes for babies born to obese mothers after gastric bypass and to specify when is the optimal time for pregnancy to occur after gastric bypass surgery.
FULL READ: Pregnancy after gastric sleeve surgery
Pregnancy after gastric bypass
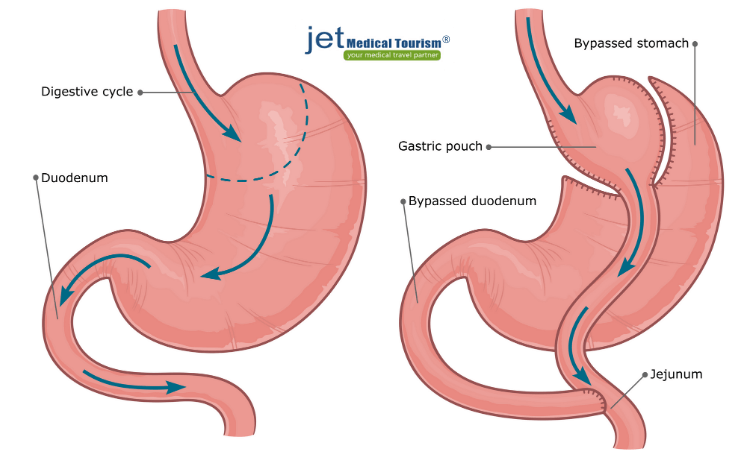
Pregnancy after gastric bypass surgery is possible and is the most advised time to get pregnant if considering bariatric surgery options. Of course, waiting a reasonable amount of time after having gastric bypass (1-2 years later) will be the safest time. There are also reports women have safely become pregnant within the first year of having done gastric bypass surgery and had successful pregnancy outcomes.
- The main benefit to having gastric bypass surgery before you decide to get pregnant (if obese) is that you can avoid many if not all of the obesity related risks of pregnancy.
- This means that if an obese person undergoes gastric bypass surgery, waits about two years and then gets pregnant, this obese person has a lower chance (or can possibly avoid) having a high-risk pregnancy in its entirely.
- This includes avoiding an “almost required” C-section that obesity would force a mother to endure.
Final thoughts on pregnancy and weight loss
Pregnancy and weight loss can seem like a difficult combination of events to happen. However, consulting your healthcare provider can help you better understand when the time is best for you to lose weight. From the first breath they take, hearing them cry out softly when they lay on your chest, to the moment they grasp your finger with their tiny fist, your baby needs you. Mothers often make sacrifices beyond belief to support their children and their needs, while at the same time mothers have unmet needs of their own.
We have to remember that if we cannot take care of our own health, we will not be around long enough to take care of our children, who are our world, meaning everything to our livelihood and happiness. When you think of how hard it is to lose weight, when you look at your growing child at home, ask yourself “Can I really delay weight loss intervention any longer?”.
“What will happen to my child, if something happened to me because of my weight?”. We’re here for you and we hear you. Here at Jet Medical Tourism®, we are ready to help you conquer your weight loss journey. Contact us today when you are ready to take the first step!
References:
- Mayo Clinic. Pregnancy week by week:-Pregnancy and obesity: Know the risks. 2020. Web. Accessed: 11. Nov, 2020. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy-and-obesity/art-20044409
- National Heart Lung and Blood Institute, NIH. Calculate your body mass index. 2020. Web. Accessed: 11, Nov, 2020. https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
- American College of Obstetricians and Gynecologists. Obesity and pregnancy. Accessed: 11, Nov. 2020. https://www.acog.org/womens-health/faqs/obesity-and-pregnancy
- Centers for Disease Control and Prevention, CDC. Defining Adult Overweight and Obesity. 2020. Web. Accessed: 11, Nov. 2020.
- McAuliffe, F. M., Killeen, S. L., Jacob, C. M., Hanson, M. A., Hadar, E., McIntyre, H. D., Kapur, A., Kihara, A. B., Ma, R. C., Divakar, H., & Hod, M. (2020). Management of prepregnancy, pregnancy, and postpartum obesity from the FIGO Pregnancy and Non-Communicable Diseases Committee: A FIGO (International Federation of Gynecology and Obstetrics) guideline. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics, 151 Suppl 1(Suppl 1), 16–36. https://doi.org/10.1002/ijgo.13334
- Tobah, Yvonne Butler, MD. The Mayo Clinic. Getting Pregnant: What do I need to know about pregnancy after gastric bypass surgery? Will my baby be able to get enough nutrients? Web. Accessed: 11, Nov. 2020.
- Dolin CD, Chervenak J, Pivo S, Ude Welcome A, Kominiarek MA. Association between time interval from bariatric surgery to pregnancy and maternal weight outcomes. J Matern Fetal Neonatal Med. 2019 Nov 13:1-7. doi: 10.1080/14767058.2019.1683156.
- Dilday J, Derickson M, Kuckelman J, Reitz C, Ahnfeldt E, Martin M, Paul Sanders J. Sleeve Gastrectomy for Obesity in Polycystic Ovarian Syndrome: a Pilot Study Evaluating Weight Loss and Fertility Outcomes. Obes Surg. 2019 Jan;29(1):93-98. doi: 10.1007/s11695-018-3473-8.
- Charalampakis V, Tahrani AA, Helmy A, Gupta JK, Singhal R. Polycystic ovary syndrome and endometrial hyperplasia: an overview of the role of bariatric surgery in female fertility. Eur J Obstet Gynecol Reprod Biol. 2016 Dec;207:220-226. doi: 10.1016/j.ejogrb.2016.10.001.
- Zeratsky, Katherine. Mayo Clinic. Has the HCG diet been shown to be safe and effective? Accessed: 11. Nov. 2020. https://www.mayoclinic.org/healthy-lifestyle/weight-loss/expert-answers/hcg-diet/faq-20058164.
- Kominiarek M. A. (2011). Preparing for and managing a pregnancy after bariatric surgery.Seminars in perinatology,35(6), 356–361. https://doi.org/10.1053/j.semperi.2011.05.022
- Rosenfield, R. L., & Ehrmann, D. A. (2016). The Pathogenesis of Polycystic Ovary Syndrome (PCOS): The Hypothesis of PCOS as Functional Ovarian Hyperandrogenism Revisited.Endocrine reviews,37(5), 467–520. https://doi.org/10.1210/er.2015-1104