Obesity and Cancer
Obesity and cancer have a known relationship. Influencing metabolic and hormonal changes, obesity works to increase DNA damage and cancer risk. Obesity ignites inflammation in the body, along with causing oxidative stress in cells, which leads to hyperplasia. Chronic inflammation suppresses the immune system, stimulating the growth of obesity related cancers. Some cancers may not be directly related to being caused by obesity, but only at aggressive levels can be related.
One example is prostate cancer which is not predominantly obesity related but can start as BHP, benign prostate hyperplasia (major risk factor for cancer) and is linked to obesity in more aggressive cancer forms. In women, endometrial hyperplasia can lead to increased estrogen levels, increasing the risk for polycystic ovarian syndrome (PCOS), and a risk factor for endometrial cancer.
Risk factors for obesity can include lack of sleep or exercise, pre-existing medical conditions such as hypothyroidism, and even genetic conditions that predispose people to obesity such as inheritable gallbladder issues. There are many types of obesity related cancers since obesity risk factors are prevalent and have been studied in the US.
Knowing science has abundantly linked obesity to causing cancer, the choices we make today influence our overall survival outcomes. Everyday prevention methods can give mixed results, however, there is hope with bariatric surgery. Contact Jet Medical Tourism® today.
Obesity causes cancer: True or False?
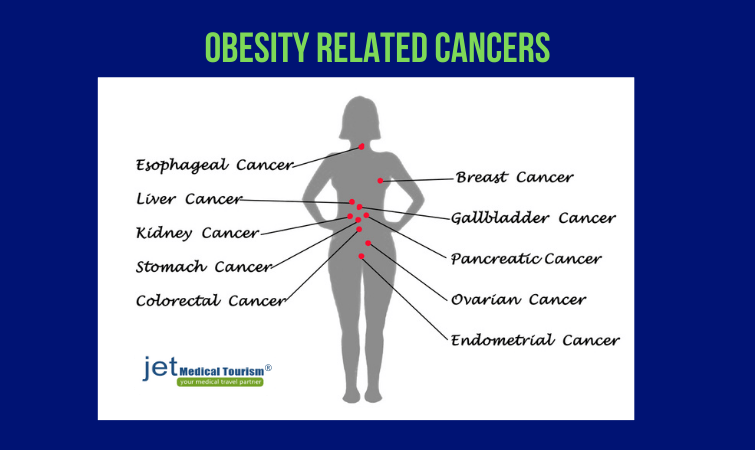
Obesity causes cancer: True! Besides obesity causing several other comorbidities such as diabetes, high cholesterol, high blood pressure, respiratory difficulties, renal disease, heart disease, gallstones, and more, obesity is also linked to cancer. Obesity related cancers may include:
- kidney
- liver
- breast
- colon/rectum
- pancreas
- thyroid
- endometrium/ovarian
- stomach (upper portion)
- meningioma (in the brain/spinal cord)
- esophagus (adenocarcinoma)
- multiple myeloma (cancer of the blood cells), and more
How does obesity cause cancer?
“How does obesity cause cancer?” you may ask. Obesity, defined at or above a 30 kg/m2 BMI/ body mass index, causes cancer since the growing abundance of fat cells in the body can stimulate a process called hyperplasia. Hyperplasia is when the number of body cells increases, thereby increasing an organ or surrounding tissue the cells comprise. Excess nutrients trigger inflammation in metabolic tissues (e.g., fat) which act as energy sources.
Fat cells secrete cytokines (regulatory messenger cells of the immune system) causing inflammation, hypertrophy (cellular enlargement) and activating cell signaling pathways that experience disruptions due to an overproduction of cytokines. Cell signal pathway disruptions can turn genes/hormones off or on and stay that way indefinitely, which can allow for tumor growth factors (increasing cancer filtration to blood vessels/angiogenesis, metastasis/spread, etc).
Obesity and cancer statistics
Obesity and cancer statistics in the US are ever growing. In the US today, Obesity affects around 40% of adults and 20% of children. The American Institute of Cancer Research/World Cancer research fund reports obesity to cause over 120,400 annual cancer cases in the US.
- The NIH reports Black adults (non-Hispanic) show the highest obesity related cancer prevalence, 38.6%.
- Hispanic adults exhibit 32.6%, while Whites (non-Hispanic) have a 28.6% obesity prevalence increasing their risk for cancer.
Obesity and cancer study
Obesity and cancer study has promoted a higher level of obesity awareness in the public. A study, CPS II, or the cancer prevention study II, was done to analyze more than one million US adults between the years 1982 and 1996. This study examined the impact of BMI on cancer mortality.
- CPS II reported most obese people (both genders) have a 40% to 80 % risk of cancer death.
- A 16-year follow-up was done on this study to further confirm a linear (increasing) relationship exists between BMI and increasing cancer mortality across most obesity cancer types.
Obesity and cancer risk
Obesity and cancer risk are intertwined as obesity is not only associated with causing cancer, but poorer survival rates from cancer. In addition, once cancer has been diagnosed, obesity also causes difficulty in detection methods and demonstrates poorer outcomes in response to treatment options.
- Between the years 1986 and 2006, 20% of all US deaths reported were caused by obesity (including obesity cancer).
- Cancer invasiveness or grade often increases with obesity in women pre- and post-menopausal.
- Triple negative breast cancer (most dangerous/aggressive subtype) is linked to obesity.
Obesity and cancer facts
Obesity and cancer facts are abundantly growing as obesity remains a pandemic. More women than men die from cancer obesity.
- Between 1986 and 2006, 20% of women died from cancer related obesity compared to 14% of men.
- As a person’s BMI increases, their risk for obesity related cancer increases, which increases their mortality risk.
- Obesity causes cancer by bringing on inflammation, hormonal changes, metabolic dysregulation, and cellular enlargement or massive cell division.
Obesity and breast cancer
Obesity and breast cancer have long been associated together with an increase in the risk of death. Obesity leads to a poorer clinical outcome in breast cancer patients. Metadata analysis was done for 82 studies, identifying 213,075 survivors of breast cancer with 23,182 deaths from breast cancer. BMI before diagnosis was compared to women of normal weight and a summary of relative risk was calculated.
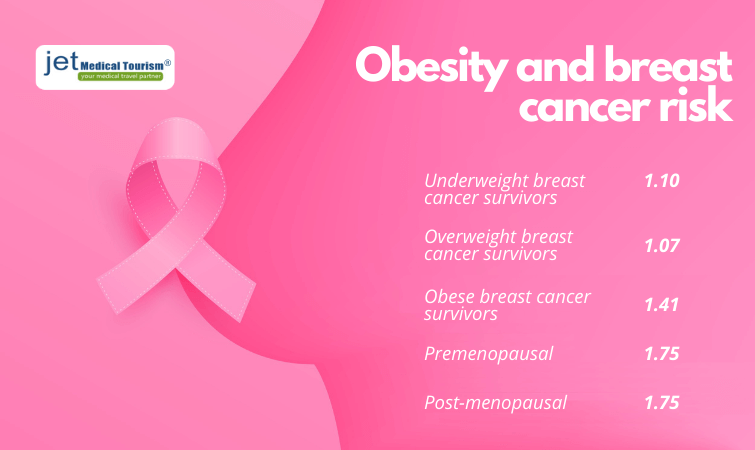
- For underweight breast cancer survivors, the relative risk for total mortality was 1.10.
- For overweight breast cancer survivors, relative risk was 1.07.
- For obese breast cancer survivors, relative risk was 1.41.
- Premenopausal relative risk was 1.75 in obese women.
- Post-menopausal relative risk was 1.34 in obese women.
Link between obesity and breast cancer
Link between obesity and breast cancer is heavily impacted in both pre- and post-menopausal women. Increasing BMI is significantly linked to breast cancer mortality. Biomarkers are commonly implicated in specific cancer types to foresee individual patient cancer risk probability. In breast cancer, ER (estrogen receptor), PR (progesterone receptor), and HER2 (human epidermal growth factor 2) are often assessed.
RELATED: Jet Medical Tourism cites US Study shows bariatric surgery may reduce breast cancer risk
Obesity and breast cancer recurrence
Obesity and breast cancer recurrence is commonly affiliated since obese women have hormonal imbalances. Hormonal imbalances can affect cancer severity and thus can progress, influencing recurrence. For example, elevated circulating leptin (appetite regulating hormone for satiety) levels in obese women account for a poorer prognosis. Adiponectin, a hormone made from fat cells to decrease inflammation and improve insulin sensitivity, is also found in low levels in breast cancer.
Obesity related cancers
Obesity related cancers often develop over time, affecting different organs, and can affect men and women differently. For example, obesity presents a moderate risk of developing colorectal cancer; obesity linked colorectal cancers in women account for 20.8% of cases, while in men, obesity linked colorectal cases are about 35.4%.
- This suggests colorectal cancer linked obesity is more common in men. Other obesity linked cancers can have different prevalence.
- Relative risk for disease mortality was compared for women with a normal BMI to women with elevated BMIs.
- For women with a BMI of 30 to <35, relative risk is 2.53.
- Women with a BMI of 40+, relative risk is 6.25.
Obesity and lung cancer
Obesity and lung cancer are not commonly linked together, but linked via the presence of smoking which exacerbates the mortality risk. Lung cancer can include many tissue (histological) types such as squamous cell carcinoma, adenocarcinoma, or small cell lung cancer. However, a study in 2019 found lipid (fat) changes in metabolism can cause oxidative stress in cells, leading to chronic inflammation and lung cancer.
Liver cancer and obesity
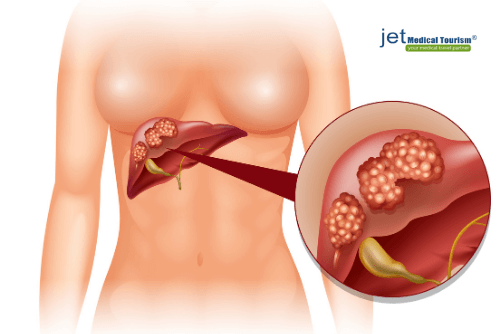 Liver cancer and obesity are commonly associated with non-alcoholic fatty liver disease, or NAFLD, which is a chronic liver disease. NAFLD commonly develops into NASH, or non-alcoholic steatohepatitis (i.e., liver buildup of fat and inflammation), then cirrhosis, and eventually cancer.
Liver cancer and obesity are commonly associated with non-alcoholic fatty liver disease, or NAFLD, which is a chronic liver disease. NAFLD commonly develops into NASH, or non-alcoholic steatohepatitis (i.e., liver buildup of fat and inflammation), then cirrhosis, and eventually cancer.
- A European study concluded NAFLD was prominent in 94% of obese people, of whom 25% had NASH.
- A study reported a 4.5 times greater risk of death in men with a BMI of 35+ than compared to men within a normal BMI range.
- Worldwide, liver cancer accounts for being the 9th most common cancer in women and the 5th most common cancer in men.
Obesity and kidney cancer
Obesity and kidney cancer are linked via insulin resistance, growth factors, and steroid hormonal imbalances. Adiponectin and growth factors such as IGF (insulin growth factor) contribute to causing kidney cancer. High blood pressure, a common obesity comorbidity, can also contribute to kidney cancer. Obese individuals also have two times the risk of developing renal cell cancer than compared to healthy weight individuals.
Obesity and pancreatic cancer
Obesity and pancreatic cancer are linked due by high level insulin production changes in the pancreas. Obesity increases the risk of developing type II diabetes, which in turn increases the risk of pancreatic cancer. According to the National Cancer Institute of the NIH, there are 30.3 million US adults living with diabetes.
- Among those, 1 in every 100 people are expected to be diagnosed with pancreatic cancer in the next three years.
- In 2019, the NIH reported 56,770 new US pancreatic cancer cases with 14,000 of those cases recently diagnosed with diabetes.
RELATED: Why does obesity cause diabetes
Obesity and uterine cancer
Obesity and uterine cancer are linked by hormonal imbalances. Specifically, elevated estrogen levels with low progesterone production due to endometrial hyperplasia can lead to uterine cancer. Endometrial hyperplasia is a condition where the inner lining of the uterus becomes too thick due to a buildup of many cells.
- Obesity causes about 57% of all endometrial cancers in the US.
- The American Institute for Cancer Research did a study that analyzed metadata from 26 studies to conclude a 50% increase in endometrial cancer risk exists with every elevation of just 5 BMI units.
Obesity cancer and depression
Obesity cancer and depression are related, especially in endometrial cancer where obesity causes poor sleep, leading to higher depression levels. Cancer survivors commonly have sleep disorders, which impact their quality of life. Harvard Medical School reports lower energy and motivation can lead to decreased activity and exercise in depressed people causing obesity.
Cancer and obesity: What you can do?
Cancer and obesity can be prevented by everyday lifestyle changes such as diet and exercise, but what happens when everyday changes just aren’t enough? Well in many people, especially those with genetic obesity (hormonal driven), weight loss cannot be successfully achieved with diet and exercise alone.
People often require bariatric surgery as the sole method for achieving long-term weight-loss due to numerous failures endured from Yo-yo dieting. Furthermore, very few studies have reported a positive relationship between having an exercise regime and achieving breast cancer survival. Maintaining long-term weight loss is key to cancer and obesity prevention.
Can bariatric surgery avoid obesity cancer?
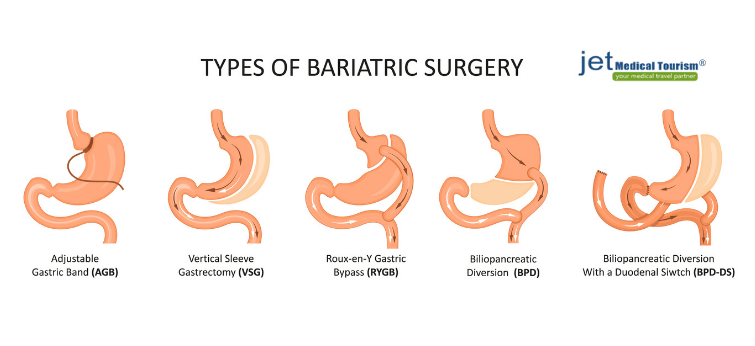
“Can bariatric surgery avoid obesity cancer”? you may ask. The answer is yes! The NIH, or National Institute of Health, reports bariatric surgery has reduced the risk of many types of cancers in obese patients when studied against other obese patients who have not had bariatric surgery performed. Among bariatric patients, cancer risk reduction was reduced in: colon, breast, pancreatic, and endometrial cancers most significantly.
Since obesity commonly causes comorbidities, such as diabetes and heart disease, it is no surprise obesity causes cancer and bariatric surgery can avoid obesity cancer. Especially since in stomach cancer, which commonly forms in the upper portion of the stomach in obese, which is the major ghrelin (hunger hormone) generator region of the body. If the upper stomach is removed via bariatric surgery, this will certainly avoid the development of obesity cancer in this hotspot.
Many studies have analyzed the impact of bariatric surgery on cancer incidence. Studies discovered bariatric surgery reduces the overall cancer incidence by 24% to 78% in obese individuals. Studies have also found a 46% cancer mortality reduction in obese patients after undergoing bariatric surgery.
Benefits of Bariatric surgery
| Intervention | Obesity | Obesity co-morbidities | Depression | Hormonal imbalance | Cancer risk | Cancer death |
| Bariatric surgery | Reduced | Reduced | Reduced | Reduced | Reduced | Reduced |
Conclusion
In such ever changing and unpredictable times we live in today, we can only count on our health to ensure our survival. Getting a cancer diagnosis can be devastating to ourselves and our loved ones. With all the numerous cancer types we are capable of getting from being obese alone, now is the time to act. Short-term obesity prevention methods have failed time and time again. Isn’t it time you deserve better?
With such rapid weight loss achieved in a short period of time, bariatric surgery is the answer to preventing the danger faced with one more added pound pushing you over the edge, the edge of developing cancer.
When you’re ready to prevent being one more added statistic of obesity cancer related deaths, when you’re ready to make a long-term lifestyle fix, when you’re ready to preserve your health, when you’re ready to say “Yes, I can!”, call Jet Medical Tourism® today to discover how you can prevent cancer!
Some other interesting articles for you:
- Obesity and COVID-19: What happens when two pandemics meet
- Pregnancy and obesity
- Ghrelin vs Leptin: Impact of hunger hormones on obesity
References:
- Parikesit Y, Mochtar CA, Umbas R, Hariandy Hamid ARA. The impact of obesity towards prostate diseases. 2016; Prostate International. (4);1,: 1-6. https://doi.org/10.1016/j.prnil.2015.08.001.
- Cleveland Clinic. Endometrial hyperplasia. 2020. Web. Accessed: 18, Nov. 2020. https://my.clevelandclinic.org/health/diseases/16569-atypical-endometrial-hyperplasia
- Cao Y, Giovannucci E. Obesity and Prostate Cancer. Recent Results Cancer Res. 2016;208:137-153. doi: 10.1007/978-3-319-42542-9_8.
- NIH: National Cancer Institute. Cancers associated with overweight and obesity. 2020. Web. Accessed: 18, Nov, 2020. https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/overweight-cancers-infographic
- NIH: National Cancer Institute. Obesity and Cancer: Pursuing Precision Public Health. 2020. Web. Accessed: 18, Nov, 2020. https://www.cancer.gov/research/annual-plan/scientific-topics/obesity.
- NIH: National Cancer Institute. New Onset Diabetes Cohort Sought to Unravel Complexities of Pancreatic Cancer Development. Accessed: 18, Nov. 2020. Web. https://prevention.cancer.gov/news-and-events/blog/new-onset-diabetes-cohort
- Chan, D., Vieira, A. R., Aune, D., Bandera, E. V., Greenwood, D. C., McTiernan, A., Navarro Rosenblatt, D., Thune, I., Vieira, R., & Norat, T. (2014). Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Annals of oncology : official journal of the European Society for Medical Oncology, 25(10), 1901–1914. https://doi.org/10.1093/annonc/mdu042
- Harvard Medical School; Harvard Health Publishing. Depression and obesity: Confirming the link. 2013. Web. Accessed: 18, Nov. 2020. https://www.health.harvard.edu/mind-and-mood/depression-and-obesity-confirming-the-link
- Park, J., Morley, T. S., Kim, M., Clegg, D. J., & Scherer, P. E. (2014). Obesity and cancer–mechanisms underlying tumour progression and recurrence. Nature reviews. Endocrinology, 10(8), 455–465. https://doi.org/10.1038/nrendo.2014.94
- Gallagher, E. J., & LeRoith, D. (2015). Obesity and Diabetes: The Increased Risk of Cancer and Cancer-Related Mortality. Physiological reviews, 95(3), 727–748. https://doi.org/10.1152/physrev.00030.2014
- Onstad, M. A., Schmandt, R. E., & Lu, K. H. (2016). Addressing the Role of Obesity in Endometrial Cancer Risk, Prevention, and Treatment. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 34(35), 4225–4230. https://doi.org/10.1200/JCO.2016.69.4638
- Zabłocka-Słowińska, K., Płaczkowska, S., Skórska, K., Prescha, A., Pawełczyk, K., Porębska, I., Kosacka, M., & Grajeta, H. (2019). Oxidative stress in lung cancer patients is associated with altered serum markers of lipid metabolism. PloS one, 14(4), e0215246. https://doi.org/10.1371/journal.pone.0215246
- Wilson KM, Cho E. Obesity and Kidney Cancer. Recent Results Cancer Res. 2016;208:81-93. doi: 10.1007/978-3-319-42542-9_5.
- Wang F, Xu Y. Body mass index and risk of renal cell cancer: a dose-response meta-analysis of published cohort studies. Int J Cancer. 2014 Oct 1;135(7):1673-86. doi: 10.1002/ijc.28813.