Ghrelin Hunger Hormone
Ghrelin hunger hormone summary: People often begin to feel a deep sense of hunger brought on by a rumbling of the stomach. The stomach is one of the most important digestive organs since it not only aids in the breakdown of ingested food by the mere presence of a strong acid (hydrochloric acid), but also contains a hormone called ghrelin.
- The duodenum (i.e., the initial part of the small intestine) is one area, among others, where ghrelin is produced in the body. However, it is specifically within the upper part of the stomach (i.e., the gastric fundus or the large pouch area of the stomach) where the majority of ghrelin is made in the human body.
- When ingested food begins to digest by exiting the stomach and entering the small bowel (i.e., the duodenum), ghrelin starts to be formed, which tells the brain it is time for a meal. In gastric sleeve surgery, this fundus area is the main part that is removed from the stomach.
Since ghrelin is made in other areas of the body, gastric sleeve patients will continue to feel a sense of hunger even though a large portion of the stomach has been removed. The hunger sensation felt after sleeve surgery is far less than patients’ experience prior to gastric sleeve surgery. For more information, contact us today.
Function of ghrelin
 Ghrelin is known to be mainly released from the upper lining of the stomach. This hunger hormone is known for its role in increasing appetite in the human body, thus ultimately causing people to feel the growing urge to eat or feel hungry.
Ghrelin is known to be mainly released from the upper lining of the stomach. This hunger hormone is known for its role in increasing appetite in the human body, thus ultimately causing people to feel the growing urge to eat or feel hungry.
- When ghrelin levels increase, this is mainly due to the stomach emptying itself out from the churned ingested food.
- As food begins to exit the stomach, becoming digested, ghrelin levels increase, and nutrient absorption begins to occur in the small intestine as the digested food moves down the intestines.
- Increases in ghrelin cause the brain to signal to the body that it is time to eat another meal.
The main area of the brain ghrelin acts on is the hypothalamus, which houses neurons that have roles in altering brain circuits. Ghrelin also works with the neurons (or brain cells) of other areas of the brain such as the pituitary gland and the hippocampus as well. The hippocampus has roles in learning, memory, and emotions. The anterior pituitary gland is involved with ghrelin since it works to increase the release of other additional hormones, such as the growth hormone.
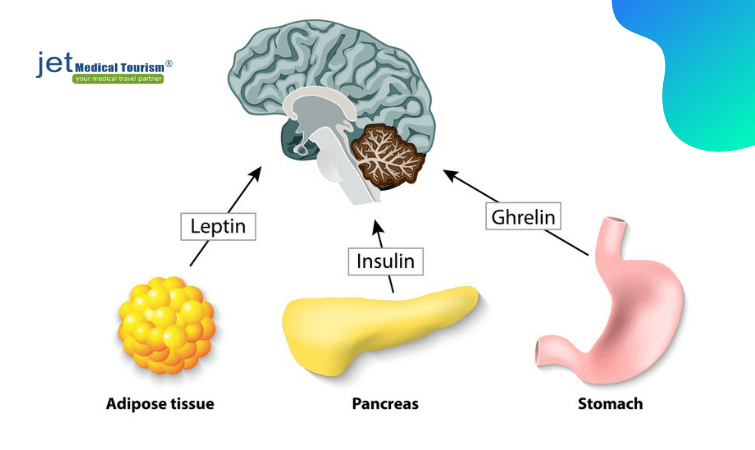
Levels of ghrelin in the blood vary before and after meals as metabolism controls the physiology, or functionality of the body systems. Ghrelin, among other hormones such as leptin (responsible for telling the body it is full; maintaining satiety), act as signal molecules in achieving an energy balance that is important for the body’s metabolism. Studies have shown leptin to have a role in controlling ghrelin to regulate appetite.
Ghrelin is also known for facilitating many other roles in the body, as it performs functions in:
- Glucose regulation
- Sleep regulation
- Promoting the taste sensation
- Increasing gut movement
- Increasing the release of the growth hormone from the anterior pituitary gland
- Increasing the release of gastric acid
- The brain’s reward system (via the dopaminergic pathway; which involves the hormone dopamine)
- Increasing fat formation (called lipogenesis), among many other functions
Mechanism of action of ghrelin
In individuals within a normal weight range, when the stomach becomes empty the body responds by producing ghrelin. Ghrelin works in response to stretch receptors in the lining of the stomach resizing its cells as food exits, where ghrelin sends signals to the brainstem.
This hunger hormone, ghrelin works to minimize energy output. Levels of ghrelin are often at their highest right before meals and lowest right after meals in healthy weight individuals. The brain works to detect when the body is in need of a meal throughout the day. Increased blood ghrelin levels cause hunger sensations to rise, telling the body more food intake is needed.
Starting in the morning of a typical day for individuals within a normal weight range:
The stomach empties=> ghrelin releases=> person feels hungry => person eats breakfast=> fat cells work to release leptin => person feels full/satiety => at lunchtime, insulin (made in the pancreas) is released from feeling hunger => person eats lunch => leptin (from fat tissues) levels increase => person feels full again => a few hours later, stomach empties again => person is hungry => ghrelin is released again => person eats dinner
Relationship between ghrelin and obesity
In obesity, the hunger hormone, ghrelin, shows an imbalance. Ghrelin blood levels do not show a drastic difference in obese individuals before and after meals, as ghrelin levels show in individuals of a normal weight range. Appetite sensation persists or can even return after an obese person has a meal because ghrelin levels tend to remain low.
Ghrelin levels tend to overall be reduced in obese individuals than compared to those within a normal weight range, it has been shown that ghrelin does not contribute to obesity, but is rather imbalanced in obese individuals.
- However, one exception to this is if a patient has an underlying genetic disorder called Prader- Willi syndrome, causing severe learning disabilities, a shortened height, among other notable features in patients.
- Prader- Willi syndrome will cause high ghrelin levels connected to increased hunger and eating, directly linked to obesity.
Since ghrelin levels remain low in the mobidly obese, this tends to trick the obese individual into believing they are staying starved. Studies have shown obese individuals show resistance to the hormone leptin, responsible for feeling full. The effects of ghrelin are opposite to that of leptin (known as an antagonistic effect).
In obesity, leptin fails to control ghrelin, thus sustaining hunger, leaving the individual unable to feel full. Ghrelin can also act on a part of the brain called the amygdala, which works in response to reward processing connected to emotional overeating.
RELATED: Ghrelin vs leptin: Impact of hunger hormones on obesity
Role of ghrelin in long-term weight loss after gastric sleeve surgery
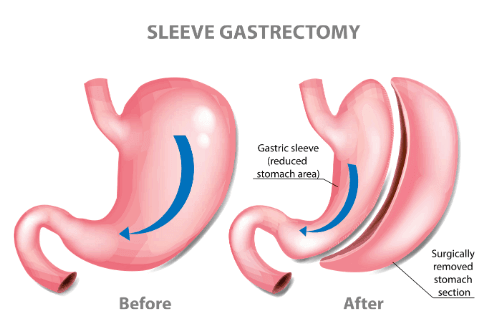 Gastric sleeve surgery has shown superior results when compared to other surgical (i.e., lap band/gastric banding, gastric bypass, etc.) outcomes in maintaining prolonged weight loss in patients. One main contributing factor to its long-term weight loss success is the fact that the main part of the stomach where the hunger hormone, ghrelin, is normally produced has essentially been removed from the body.
Gastric sleeve surgery has shown superior results when compared to other surgical (i.e., lap band/gastric banding, gastric bypass, etc.) outcomes in maintaining prolonged weight loss in patients. One main contributing factor to its long-term weight loss success is the fact that the main part of the stomach where the hunger hormone, ghrelin, is normally produced has essentially been removed from the body.
The combination of not only achieving a smaller stomach size but low ghrelin levels as well makes gastric sleeve surgery the most widely used and successful bariatric surgical option worldwide. In this surgery, the minimized sized stomach (reduced by about 80% of the patient’s original stomach size) is shaped into a sleeve.
- With less of the stomach available after sleeve surgery, the hunger signals due to minimized ghrelin levels become much weaker.
- Weaker hunger signals to the brain prevent the patient from feeling the urge to eat frequently and abundantly as they once felt prior to surgery.
How long before ghrelin comes back after gastric sleeve surgery?
About two years after the gastric sleeve surgery has been performed, it is possible for ghrelin levels to come back. However, this result is patient dependent and results may vary from patient to patient case by case. Some patients may experience an increase in ghrelin just 12 months after their gastric sleeve surgery.
Ghrelin levels can vary between males and females, levels also depend on the physiological implications of the patient as well. More studies are still underway to prove a more accurate timeline for the majority of gastric sleeve patients.
How well does the gastric sleeve remove ghrelin hunger hormone?
Gastric sleeve surgery reduces ghrelin levels by about 80%. Ghrelin will no longer be formed in the upper part of the stomach after gastric sleeve surgery, which is the main area that concentrations of the hormone ghrelin originate from in the body.
Only other minor areas of the bowel will still continue to produce ghrelin, allowing an individual after surgery to still feel some hunger. However, much of the body‘s ghrelin levels will be removed with this surgical procedure, allowing ghrelin levels to be drastically reduced after surgery.
Does the gastric sleeve surgery stop ghrelin hunger hormone production?
No, the gastric sleeve reduces ghrelin, but can not stop its production from the entire body. Ghrelin is still being made in other parts of the body (a small amount is made from the small bowel) even after gastric sleeve surgery.
Other parts of the body that produce minor ghrelin amounts are the:
- jejunum and ileum (parts of the small intestines)
- lungs
- parts of the pancreas
- placenta
- kidneys, among a few others.
This is because the gastric sleeve surgery only works to remove the main upper part of the stomach (i.e., fundus) where most of the body’s ghrelin source is made.
Does ghrelin hunger hormone come back after gastric sleeve surgery?
Yes, it is possible for ghrelin levels to return. The sleeve may become swollen, generating gastritis, or inflammation of the stomach, a while after a gastric sleeve surgery has been performed. Controlling stomach acids levels and maintaining a healthy diet can prevent ghrelin levels from returning.
However, the gastric sleeve or the laparoscopic sleeve gastrectomy (LSG or SG) which uses a minimally invasive fine camera scope for surgery remains the number one leading bariatric surgical procedure in the world, contributing to over 50% of bariatric surgeries performed in the US today due to its successful results. Sleeve gastrectomy provides patients with a decreased appetite and weight loss results.
References:
- Tortora, GJ, Derrickson, B. Principles of Anatomy & Physiology. (Fifteenth edition). 2017. Wiley: Hoboken, NJ.
- Martini, R, Ober, B, Nath, J, Bartholomew, E, Petti, K. Visual Anatomy & Physiology. (Third edition). 2018. Pearson: NY, New York.
- Raven, PH, Johnson, GB, Mason, KA, Losos, JB, Duncan, T. Biology. (Twelfth edition). 2020. McGraw Hill: NY, New York.
- Sethi, P., Thillai, M., Nain, PS., Ahuja, A., Aulakh, N., & Khurana, P. (2018). Role of Hunger Hormone “Ghrelin” in Long-Term Weight Loss Following Laparoscopic Sleeve Gastrectomy. Nigerian journal of surgery : official publication of the Nigerian Surgical Research Society, 24(2), 121–124. https://doi.org/10.4103/njs.NJS_24_17.
- Terra X, Auguet T, Guiu-Jurado E, Berlanga A, Orellana-Gavaldà JM, Hernández M, Sabench F, Porras JA, Llutart J, Martinez S, Aguilar C, Del Castillo D, Richart C. Long-term changes in leptin, chemerin and ghrelin levels following different bariatric surgery procedures: Roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2013 Nov;23(11):1790-8. doi: 10.1007/s11695-013-1033-9. PMID: 23832521.
- Parada D, D., Peña G, K. B., Vives, M., Molina, A., Mayayo, E., Riu, F., Sabench, F., & Del Castillo, D. (2020). Quantitative and Topographic Analysis by Immunohistochemical Expression of Ghrelin Gastric Cells in Patients with Morbid Obesity. Diabetes, metabolic syndrome and obesity : targets and therapy, 13, 2855–2864. https://doi.org/10.2147/DMSO.S260483.
- McCarty, TR, Jirapinyo, P, Thompson, CC. Effect of Sleeve Gastrectomy on Ghrelin, GLP-1, PYY, and GIP Gut Hormones, Annals of Surgery: July 2020 – Volume 272 – Issue 1 – p 72-80 doi: 10.1097/SLA.0000000000003614.
- Bužga, M., Zavadilová, V., Holéczy, P., Švagera, Z., Švorc, P., Foltys, A., & Zonča, P. (2014). Dietary intake and ghrelin and leptin changes after sleeve gastrectomy. Wideochirurgia i inne techniki maloinwazyjne = Videosurgery and other miniinvasive techniques, 9(4), 554–561. https://doi.org/10.5114/wiitm.2014.45437.
- Müller TD, Nogueiras R, Andermann ML, Andrews ZB, Anker SD, Argente J, et al. (June 2015). “Ghrelin“. Molecular Metabolism. 4 (6): 437–60. doi:10.1016/j.molmet.2015.03.005
- Goldstone AP, Thomas EL, Brynes AE, Castroman G, Edwards R, Ghatei MA, et al. (April 2004). “Elevated fasting plasma ghrelin in prader-willi syndrome adults is not solely explained by their reduced visceral adiposity and insulin resistance“. The Journal of Clinical Endocrinology and Metabolism. 89 (4): 1718–26. doi:10.1210/jc.2003-031118
- Iannelli A, Dainese R, Piche T, Facchiano E, Gugenheim J. Laparoscopic sleeve gastrectomy for morbid obesity. World J Gastroenterol. 2008 Feb 14;14(6):821-7. doi: 10.3748/wjg.14.821.