Obesity and COVID-19: What Happens When Two Pandemics Meet

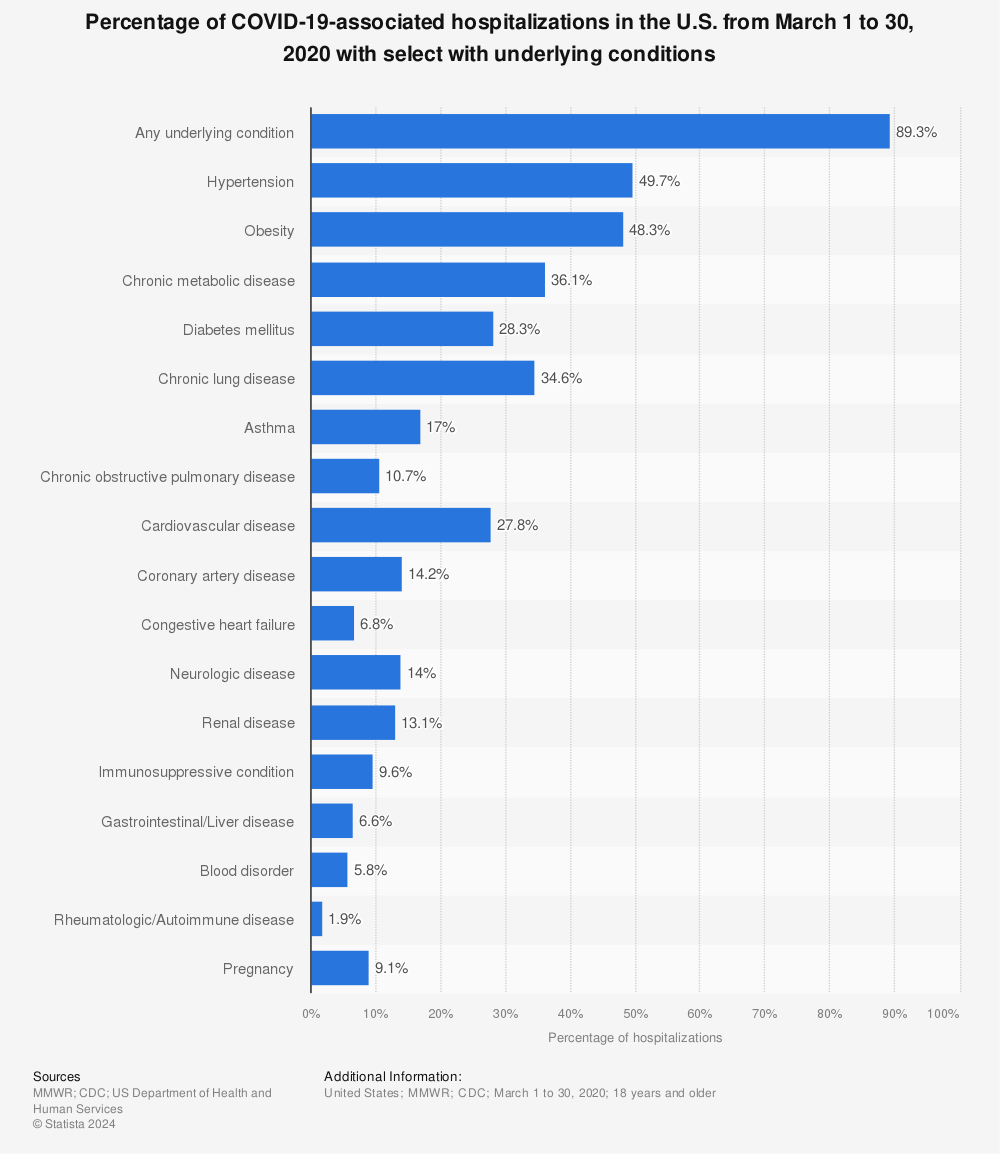
Obesity and COVID-19 in the US has taken a large toll on many Americans, especially considering how deadly is the coronavirus on those of us with pre-existing conditions. From heart disease, high blood pressure, high cholesterol, to respiratory distress, to kidney failure, to diabetes, to cancer, coronavirus or COVID-19 can threaten the lives of anyone who suffers from such pre-existing conditions even more.
To an even greater extent, people are especially vulnerable to coronavirus if they suffer from obesity or morbid obesity. This is because obesity increases a person’s chance of suffering not one, but multiple pre-existing conditions.
Obesity and COVID-19 go hand in hand in a time where people do not have much choice over their healthcare or many options to choose from if they get infected. If we can decrease our chances of being obese, we can essentially decrease our chances of contracting coronavirus since we would prevent the development of pre-existing conditions. The most at-risk group of people to coronavirus are senior citizens who are morbidly obese. This would be due to their weaker immune systems and other present pre-existing conditions morbid obesity would cause.
To learn more about obesity and COVID-19, keep reading this informative article. You can also contact Jet Medical Tourism® below.
Obesity in America
Obesity in America has been increasing in numbers over the years. Thus, increasing people’s risk of death or even depriving them of living life to the fullest.
- According to the CDC (or Centers for Disease Control and Prevention), in the year 1999 the prevalence of obesity was 30.5%.
- Obesity prevalence then increased up to 42.4% in 2018 for adults.
- Furthermore, severe obesity increased in prevalence as well, in 1999 it was only 4.7%, then jumped to 9.2% in the year 2018.
- In 2019, the obesity rate in children was 18.5% in the US.
- Obesity risk tends to increase in people with lower education and has also been associated with higher risk in people coming from lower socioeconomic backgrounds as well.
In 2018, the CDC reported only nine states to be affected by adult obesity (having 35% or more of the population obese). However, in 2019 twelve states were reported to reach 35% obesity or above. Those states are: West Virginia, South Carolina, Mississippi, Michigan, Tennessee, Kentucky, Oklahoma, Indiana, Arkansas, Alabama, Kansas, and Louisiana.
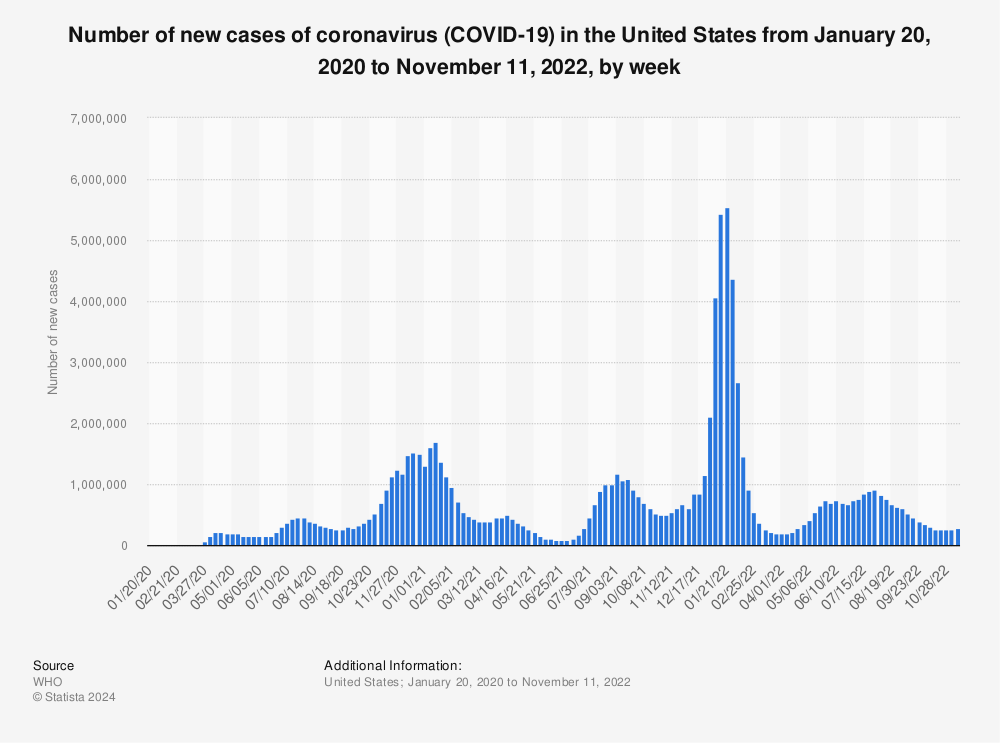
COVID-19 coronavirus in the US
COVID-19 in the US early in 2019 made us think it was only an international crisis. It started in China (city Wuhan) as a SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus, it won’t reach here, or at least that’s what we were told… The ambulances suddenly came rushing in, day by day we started to hear the sirens in our streets more and more starting in March of 2019. From then on, our hospitals became slammed, with beds reaching full capacity in the state of New York early on.
- We were told hospital staff may have to start choosing which patients can receive treatment vs which patients are not, based on the presence of pre-existing conditions and age criteria. Field camps were set up outside hospitals to support added COVID-19 beds, while bodies piled up inside chilled trucks headed for funeral homes that have no more storage. Our brave licensed, certified medical staff began to volunteer, risking their lives to treat our fellow Americans in hospitals across states, where ever the surge would hit without limits.
- Many of our medical staff remain heroes today as they lost their lives to coronavirus while fighting to save someone else. Doctors started sleeping away from their homes, avoiding their children in fear of what they may bring home to them. Nurses began making PPE (personal protective equipment) an attempt to protect themselves and their co-workers due to manufacturing shortages in supplies.
Schools closed and millions of people lost their jobs due to the economic crisis affecting company budgets, or social distancing requirements limiting the number of employees still in effect until today. People started to quarantine for two weeks straight inside their homes isolated from family members as much as possible, every time they are exposed to a positive case. With many people being out of work for so long, this made people less able to go out, less able to exercise and more likely to eat.
Dangers of obesity vs COVID-19
Dangers of obesity vs COVID-19 are similar in that both illnesses together can be even more life-threatening than if individually manifested. Obesity causes cardiovascular problems, type II diabetes, high blood pressure (hypertension), etc. Obesity serves as a high-risk factor for severe COVID-19 cases.
- According to a recent article published in the Journal of medicine, increasing morbid obesity BMI (body mass index) increases the severity or aggressiveness of COVID-19 in humans. This means the higher a person’s BMI is already if they contract COVID-19, they will have a poorer prognosis due to the virus taking a harder toll on their body, possibly killing them sooner than healthy weight individuals.
- COVID-19 is known to cause blood clots, leading to stroke, which kills people in the end just as obesity tends to do.
How Obesity is associated with severe forms of COVID-19
Obesity is associated with severe forms of COVID-19 since physiological problems become enhanced by the virus. Through cell signaling pathways, obesity causes oxidative stress on cells, disabling their function, and speeding up viral inflammation response to COVID-19.
Fat reduces the ability of our body’s immune cells to do their job in protecting us from invading infections. The greater the amount of fat tissue we have, the harder our body’s cells have to work in protecting us, which in many cases falls short, leading to increased chances of viral (and even bacterial infection) contraction.
5 Reasons why COVID-19 is more deadly in people with obesity
Reasons why COVID-19 is more deadly in people with obesity can be endless. Obesity in America continues to be an on-going problem, just as COVID-19 has been continuing to take more American lives each day. Obesity can even put people at a greater risk of influenza, which if entering the hospital with flu symptoms these days, can put an obese person more at risk from contracting COVID-19. Being hospitalized or placed on a ventilator to help patients be able to breathe easier is more common among obese patients than non-obese.
COVID-19 is more deadly in people with obesity because of how human biology affects our physiology (the function of our body):
- Obesity leads to impaired immunity, lowering our white blood cell counts. This makes our bodies more prone to infection.
- Obesity causes chronic (on-going) inflammation in certain parts of our body.
- Obesity increases cholesterol levels, which increase the chance for our blood to clot and not flow smoothly through blood vessels. COVID-19 injuries cells, making red blood cells more likely to clot, causing a stroke.
- Obese people already have heart problems, many due to diabetes type II, with high blood sugar levels, and high blood pressure.
- Obese people already have a hard time breathing due to excessive weight bearing down on the lungs with movement and COVID-19 enhances lung disease. COVID-19 reduces lung functionality, making it harder for an obese person to effectively benefit from oxygen therapy administered via mechanical ventilation.
Obesity and COVID-19 in the US vs other countries
Obesity and COVID-19 in the US have been much more severe in terms of cases and fatalities than compared to other countries.
- For example, the numbers (known as prevalence) are increasing by the day, but as of today Johns Hopkins University, JHU, reports the current number of COVID-19 cases in the US to be at 10,217,789.
- JHU reports the US death toll currently stands at 239,374.
- Italy currently has 42,330 deaths.
- China stands at 4,742 deaths.
- Italy has an obesity prevalence of 20%, China has 6%, and the US has over 40%. Mexico currently has 95,027 deaths with 36.1% obesity. This suggests the cases speak volumes, the prevalence of obesity is directly tied to the number of COVID-19 cases.
Morbid obesity and COVID-19
Morbid obesity & COVID-19 together are a very dangerous combination. Morbid obesity is when a person has a BMI of 40 (kg per meter squared units) or greater. Regular obesity is around 30 to 35. Speaking of obesity or morbid obesity, fat inside the body, if excessive, pushes the diaphragm (muscular dividing layer lining the bottom of the lungs; separates the digestive organs from the respiratory organs) in the lower area of the lungs.
- Once the diaphragm is pushed into the lower lungs, this reduces the lung capacity for breathing.
- The lower area of the lungs contains high levels of oxygenated blood than compared to the upper lungs.
- So, a diaphragm pushed into the lower lung area by excessive fat would block the lung’s access to high oxygenated blood and reduce breathing efficiency in obesity.
- Then if viral particles enter the lungs, triggering an immune response, breathing becomes almost impossible for the obese person alone to accomplish without a mechanical ventilator.
- We know that the majority of patients placed on a ventilator who are obese or morbidly obese end up dying.
RELATED READ: Morbid obesity BMI chart: Am I morbidly obese?
Obesity and coronavirus facts
Obesity and Coronavirus facts are becoming more clear day by day with all the research done throughout this year. COVID-19 has exacerbated our nation’s problem with obesity so much more. If we consider how these two pandemics merge in the body, we must understand the physiology (body function) of what is going on.
- The most vulnerable people to COVID-19 are those with a pre-existing condition (such as obesity or other comorbidities caused by obesity or even cancer).
- The high-risk group for contracting the coronavirus also includes the elderly with a weakened immune system and very young children with an underdeveloped immune system.
Obesity and COVID-19 outcomes
Obesity and COVID-19 outcomes have been analyzed in studies since the start of early 2020. In the US, patients that were less than 60 years old with a BMI in the range of 30 to 34 were tested to access their level of needed hospitalization outcomes.
- The high BMI group as described was found to be 2 times more likely to need acute care (short-term) and 1.8 times more likely to need critical care (intensive care unit; ICU) from COVID-19 than compared to people tested with a lower BMI and of similar age.
- Severely obese people tested in this study with a BMI greater than 30, similar aged, were found to 2.2 times more likely to need acute care and 3.6 times more likely to require critical care services than compared to people with a lower BMI (less than 30).
Obesity and COVID-19 mortality
Obesity and COVID-19 mortality are directly related since as the level of obesity increases, the risk of COVID-19 mortality also increases. Studies have shown COVID-19 deaths to be commonly associated with obesity and even more deaths have been reported with morbid obesity. This includes obese people who have no other pre-existing or underlining conditions (i.e., diabetes), deaths have been reported connecting only obesity and COVID-19 as well.
A New York study examined 5,700 patients with an average age of 63 years old. The participant’s pre-existing conditions included: 41.7 % of the group had diabetes, 56.6% had hypertension, and 41.7% had only obesity (with no other comorbidities). Among this study group:
- 3.2% of patients were given kidney replacement therapy.
- 12.2% of the participating patients required a ventilator for breathing.
- The death total of the group was 21%.
- Within the group of patients placed on a ventilator, 88.1% of those patients had all died. This suggests the majority of patients who will be placed on a ventilator have a high risk of death, especially if they have obesity or other pre-existing conditions.
Impact of COVID-19 on bariatric surgery
Impact of COVID-19 on bariatric surgery has caused clinicians to recommend delaying any form of elected surgery until the pandemic subsides. Once COVID-19 cases decline enough it will be safer for patients, especially those morbidly obese to resume bariatric surgery options. Jet Medical Tourism® offers bariatric surgical services that take place in Mexico, where there is a much lower risk for contracting COVID-19 than compared to here in the US.
Certain patients with advanced obesity comorbidities (arising conditions) such as type 2 diabetes, renal failure, or those in need of time-sensitive organ transplants may be at greater harm from delaying bariatric surgery. It is recommended all patients consult with a physician regarding bariatric surgical options to understand when they may be deemed safe to access depending on the urgency of their current health situation and medical history.
YOU MIGHT ALSO LIKE: Impact of Coronavirus (COVID-19) on medical tourism
Recommended Bariatric Surgery Access:
| Access | Time | Patient Criteria |
| Urgent | <30 days | Patients present severe symptoms/complications which will quickly deteriorate. |
| Expedited | <90 days | Patients present risk of harm with organ transplant/complex medical case, which is deteriorating. |
| Standard | >90 days | Patients present mild dysfunctions unlikely to deteriorate within 6 months of delayed surgery. |
Steps an obese person should take amid two pandemics
Steps an obese person should take amid two pandemics to stay safe include consulting with their physician on when may be best to undergo any interventions for weight loss and continue to demonstrate social distancing.
- Another helpful step during this time is to stay home as much as possible if you are obese, avoiding large gatherings of people.
- Wearing a mask when in the presence of other people helps prevent the spread of COVID-19.
- Weight loss interventions that are most effective in achieving rapid long-term weight loss include bariatric surgery. If an obese person attempts to lose weight during this pandemic of COVID-19, it can lower their risk of contracting the virus.
- By reducing the risk of viral contraction, obese people can save their lives and live longer. However, we must remember to exercise caution to first understand when the timing may be right for any bariatric surgery this year or next year, depending on our specific health situation.
Pro Tip:
As a pro tip to stay aligned with your health while waiting for bariatric surgery to be deemed safe again, patients can try to eat a nutritious diet within the lower glycemic index (leafy greens such as spinach, kale and high protein such as chicken breasts, etc). Patients can also:
- Be sure to practice glycemic control and daily monitoring, if diabetic
- Continue to take all medications as prescribed by your physician
- If a physician recommends your wait time be extended due to COVID-19, ask about drug intervention options for weight control, which may temporarily improve your health.
Final words
We all come from different backgrounds, different homes, different cultures, different levels of education or industries, but in the end, we must ask ourselves “Do we all just want the same thing?”. We all want to be safe, live a healthy lifestyle and most importantly, live the longest lifespan we can. With all that is going on these days and the unknown, we have to think more about our health, our choices, and our future.
Whether you live alone, with your family, or still like to make a growing family of your own someday, we need to fight this epidemic of obesity and not let ourselves succumb to being one of the growing statistics of Americans lost to the greater pandemic of the coronavirus.
Many obese or morbidly obese people struggle to find work and keep a career due to their health issues or limitations. Maybe you’re a single mom who has young children at home, whose future depends on you and your decisions. Maybe you’re a single dad just trying to protect your kids and be more involved in their lifestyle choices. Maybe you have a family who needs you to work every day to support them to continue to provide for your livelihood and theirs.
The future is now, it is happening now, it is happening with our choices. Let us work together to defeat obesity and protect ourselves from the coronavirus. Remember, it all starts with you. Contact Jet Medical Tourism® today to learn more about how you can overcome obesity and improve your health with bariatric surgery; and become better protected from the coronavirus!
References:
- Centers for Disease Control and Prevention. Adult Obesity Facts. (2019). Web. Accessed: 9. Nov, 2020. https://www.cdc.gov/obesity/data/adult.html
- Wadman, Meredith. American Association for the advancement of science. Why COVID-19 is more deadly in people with obesity- even if they are young? (2020). Web. Accessed: 9, Nov. 2020. https://www.sciencemag.org/news/2020/09/why-covid-19-more-deadly-people-obesity-even-if-theyre-young
- Caci G, Albini A, Malerba M, Noonan DM, Pochetti P, Polosa R. COVID-19 and Obesity: Dangerous Liaisons. J Clin Med. 2020 Aug 4;9(8):2511. doi: 10.3390/jcm9082511.
- Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., Barnaby D.P., Becker L.B., Chelico J.D., Cohen S.L., et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020;323:2052. doi: 10.1001/jama.2020.6775
- Johns Hopkins University & Medicine. COVID-19 dashboards by the center for systems science and engineering (CSSE) at Johns Hopkins University (JHU). 2020. Web. Accessed: 10, Nov. 2020. https://coronavirus.jhu.edu/map.html
- Pearce, Katie. Johns Hopkins University. Obesity a major risk factor for COVID-19 hospitalization. 2020. Web. Accessed: 10, Nov, 2020. https://hub.jhu.edu/2020/06/01/david-kass-obesity-covid-19/
- Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) requiring invasive mechanical ventilation. Obesity (Silver Spring)2020; 28: 1195‐ 1199.
- Barquera, Simón and Rivera, Juan A. Obesity in Mexico: rapid epidemiological transition and food industry interference in health policies. The Lancet. Diabetes & Endocrinology;2020; (8)9: 746-747. https://doi.org/10.1016/S2213-8587(20)30269-2.
- Rubino, F., Cohen, R. V., Mingrone, G., le Roux, C. W., Mechanick, J. I., Arterburn, D. E., Vidal, J., Alberti, G., Amiel, S. A., Batterham, R. L., Bornstein, S., Chamseddine, G., Del Prato, S., Dixon, J. B., Eckel, R. H., Hopkins, D., McGowan, B. M., Pan, A., Patel, A., Pattou, F., … Cummings, D. E. (2020). Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritisation of access to surgery. The Lancet. Diabetes & Endocrinology, 8(7), 640–648. https://doi.org/10.1016/S2213-8587(20)30157-1.